Foot injuries make up a not insignificant proportion of sports injuries, but the kind of frequency varies depending on the sport. According to the 2018 Sports Report of the Verwaltungs-Berufsgenossenschaft (VBG), basketball accounted for 7.4 % of foot injuries, ice hockey for 5.6 %, football for 10.3 % and handball for 4.3 % [20]. Metatarsal fractures are the most common entity [3]. The first metatarsal is the least commonly fractured, accounting for approximately 5 % of metatarsal fractures, and the fifth metatarsal the most commonly fractured, accounting for approximately 56 %. Fractures are evenly spread among the other metatarsals [6]. Stress fractures may occur as well as traumatic fractures. They account for 38 % of stress fractures of the lower extremity. Stress fractures mostly involve the second and third metatarsals [6]. Irrespective of whether an acute or stress fracture is present, it is essential to identify as soon as the cause and contributory risk factors as quickly as possible factors. Subsequent treatment should take these into account.
Symptoms
Whereas in acute fractures sudden onset of pain is typically a cardinal symptom, in metatarsal stress fractures it generally develops gradually. Reduced loading capacity is associated with fractures irrespective of aetiology. Adequate early diagnosis and identification of risk factors are particularly detraining important in competitive sports to avoid long periods without training or competition.
Risk factors
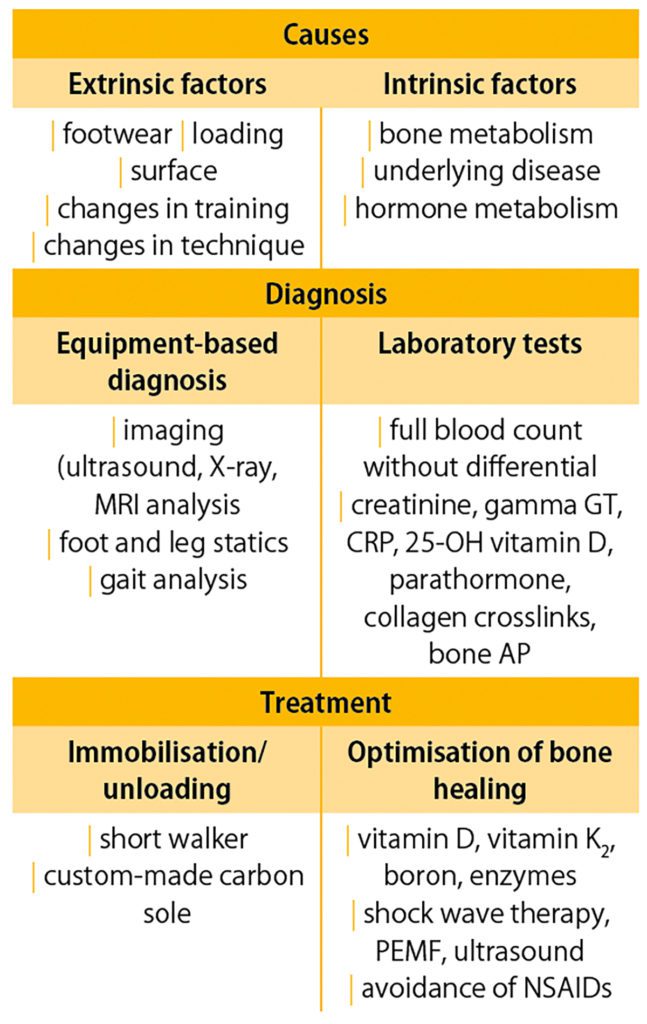
It is crucial to identify any predisposing factors. For example, stress fractures are more common in ballet dancers due to repeated maximum plantar flexion [36, 27]. Athletes in sports with high running or jumping loads are also at risk. As retiring from the sport is not an option for competitive athletes, it is essential to identify other possible causes. These may include changes in loading, such as increased training volumes, changes in surface, new shoes, special shoe inserts or biomechanical compensation mechanisms following prior injury [7, 21]. Systemic causes should also be considered. These include changes in hormone balance, eating disorders and malabsorption syndrome [1, 2]. The female athlete triad is a common example [33, 1]. It is therefore important to check intake of protein, calcium and vitamins D and K2, as well as use of alcohol, opioids and tobacco [28, 10]. Nonsteroidal anti-inflammatory drugs (NSAIDs) in particular can have a negative impact on fracture healing. Use of NSAIDs has caused a significant decrease in trabecular bone mass in ectopic ossification areas due to the decreased number and activity of osteoblasts. This is caused by interference with the bone morphogenetic protein-7 (BMP-7) signalling pathway. Although trauma is the direct cause in acute fractures, the other above factors can predispose to fracture and should therefore also be considered even if the immediate cause is apparent. [32]
Diet
Diet can have both a positive and negative effect on fracture healing. First, it is essential to avoid any toxins. Smoking and heavy drinking are associated with loss of bone mass (osteopenia) and increased risk of fracture [28]. The available data on moderate drinking is still inconclusive [38]. In general, a fully nutritious diet is essential in any injury to ensure an adequate supply of energy and protein. In this case, 2 – 2.5 g protein / kg body weight are recommended. It is especially important to prevent micronutrient deficiencies. Vitamins D and K2, magnesium and boron are particularly important in promoting bone healing.
Vitamin D deficiency
Vitamin D plays an important role in calcium and phosphate homeostasis. Particularly in combination with calcium it helps maintain a balanced bone metabolism [18, 19]. It is therefore essential to rule out vitamin D deficiency (< 25 nmol/L) [9] and any possibility of resulting secondary hyperparathyroidism (sHPT). Prolonged sHPT is associated with impaired bone turnover [23, 17] and can also lead to loss of mineral salts [26, 17]. Guidelines recommend measurement of 25-hydroxy vitamin D serum levels in all patients with sHPT [22].
Osteopenia
Osteopenia can occur alone or as a result of vitamin D deficiency [17]. Diagnosis mostly involves dual-energy X-ray absorptiometry (DXA). A new procedure will allow bone density to be determined without the need for exposure to radiation based on calcium homeostasis in the skeleton [9].
Biomechanical compensation mechanisms
If the above mentioned risk factors have been ruled out or recurrent metatarsal injuries occur, structural compensation mechanisms should also be considered [8]. These mechanisms can result in an imbalance in the loading and unloading of bones and soft tissue structures, resulting in fracture [21]. From a biomechanical perspective, changes in movement vectors and the resulting force vectors lead to incorrect loading e.g overloading [31]. A picture of the movement pattern and the resulting loading vectors can be gained using gait/running analysis, which allows the kinematics and kinetics of the lower extremity to be observed [5]. Use can also be made of dynamic procedures such as foot pressure measurement and gait analysis [7, 5, 11]. These allow observation of, for example, running and foot roll behaviour.
Based on the findings, it is possible to counteract incorrect biomechanical and compensation loading with the choice of individual shoe inserts and foot muscle training
Diagnosis
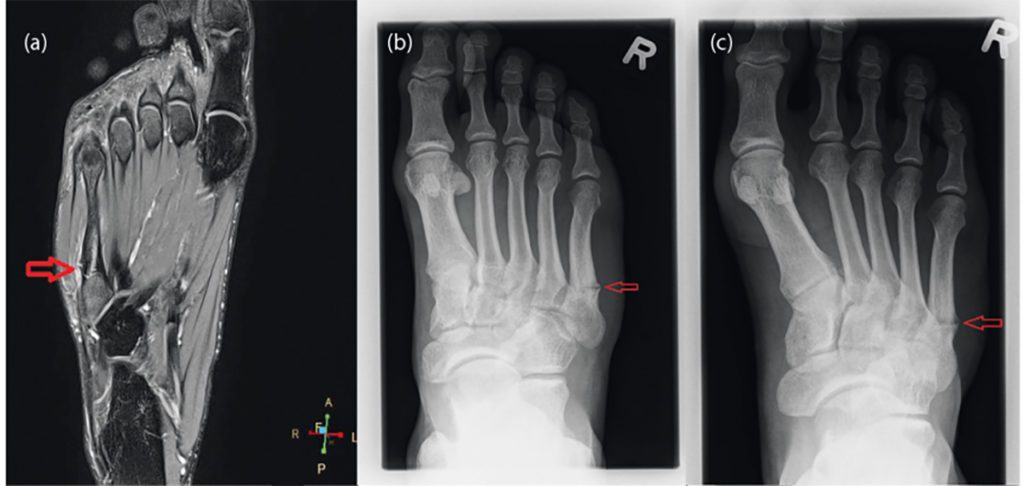
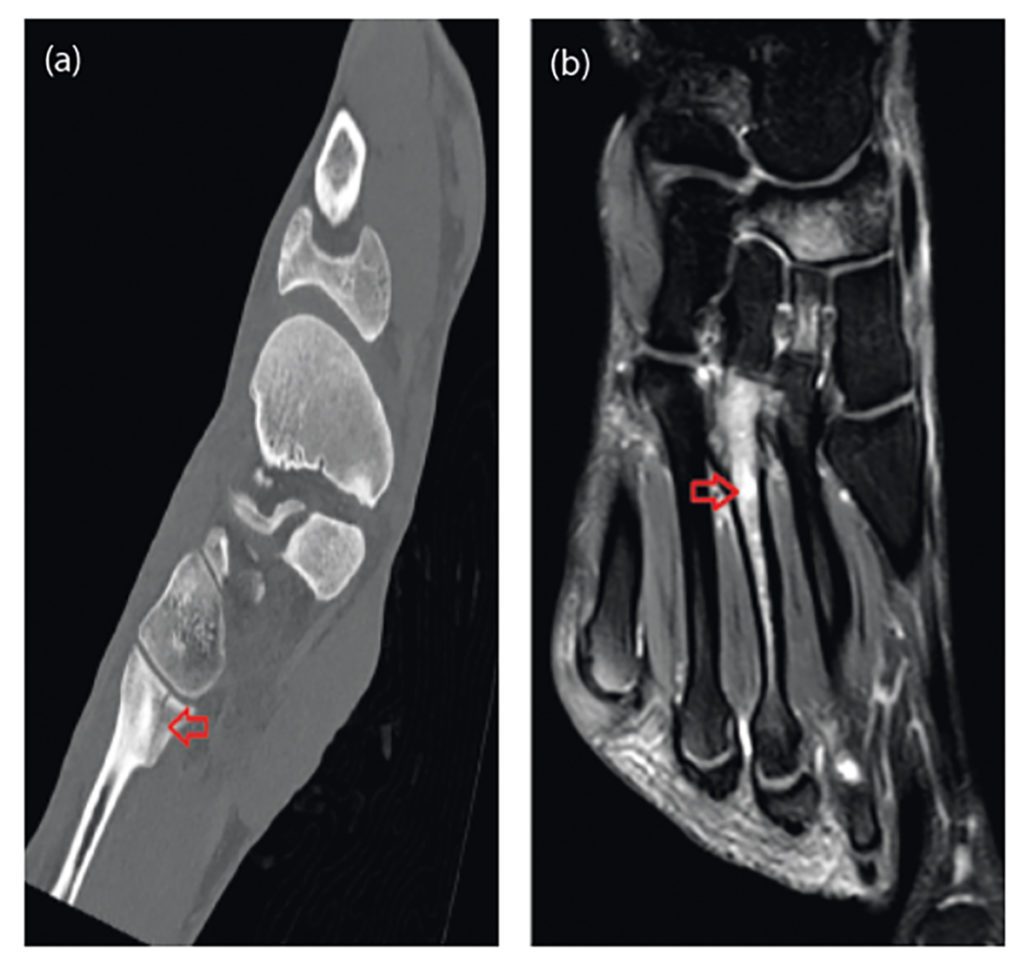
Following medical history and physical examination, it is advisable to perform diagnostic ultrasound of the foot to gain a more better understanding of the fracture. In the hands of an experienced investigator, diagnostic ultrasound is just as sensitive and specific as diagnostic X-ray [4]. However, if a fracture is suspected, this should be followed by diagnostic X-ray of the foot in three planes [3]. In fractures of the base of metatarsals 1 – 4, computer tomography should also be performed, as such fractures may be associated with Lisfranc dislocation fractures. In the case of stress fractures, MRI is the gold standard, as X-ray images are often falsely negative [36].
Treatment
Conservative or surgical treatment
Shaft fractures of metatarsals 2 – 5 with no or slight dislocation can be treated conservatively. Dislocations of up to 3 mm and plantar malalignment up to 10° are amenable to conservative treatment [3]. In such cases, immobilisation in a short walker with full weight bearing adjusted according to pain level is sufficient. This treatment when combined with a change of shoe to one with a rigid sole after 4 – 6 weeks has the advantage of a better functional outcome compared with immobilisation in a lower leg plaster cast [4]. Provision with a carbon sole is also a primary consideration. Fractures of the first metatarsal with dislocation should be surgically stabilised, as this bone plays a central role in carrying body weight and in the foot arch [4]. Fractures of more than one metatarsal, even with slight dislocation, require surgery [3]. In subcapital and metatarsal head fractures, axial deviations up to 10o are similarly amenable to conservative treatment.
Conservative treatment consists of unloading the forefoot by means of a rigid sole with full weight bearing adjusted according to the pain level. For fractures with greater dislocation and extra-articular fractures, intramedullary wires are the fracture-fixation procedure of choice [3]. Surgery should also be indicated for shortened metatarsals or rotation defects of the toes [12].
Special features of stress fractures
Stress fractures commonly involve the neck of the second and third metatarsal and the shaft of the fifth metatarsal. A very pronounced foot arch increases the risk of stress fractures of the fifth metatarsal due to increased loading [12]. It can take 3 – 6 months for the fracture to heal. As with traumatic fractures, treatment consists of initial unloading with gradual restoration of weight bearing as the bone heals [15]. Stress fractures of the fourth and fifth metatarsal in particular are more prone to non-union [36]. In a case series, 11 athletes with stress fractures of the base of the fourth metatarsal were therefore treated with plate fixation and autologous bone grafting from the calcaneus. On average, all athletes were able to return to sports after 12 weeks [30].
Procedures to promote bone healing
Non-union may occur with both acute and stress fractures. There are various treatment procedures that may be used before surgical revision needs to be considered. It is essential not to delay their use until it is too late but to initiate application as early as possible in the healing process.
Shock wave therapy
Shock waves ensure increased production of growth factors, nitrogen oxides and free radicals, which trigger the healing process. This can be exploited to treat stress fractures [15]. Shock wave therapy induces angiogenesis, and mesenchymal stem cells differentiate to osteoblasts. The periosteum is also stimulated, which plays a major role in callus formation [15]. There are a number of case series that report positive outcomes for stress fractures. These involved the use of focused medium to high energy shock waves.
In most cases the same doses were used as for non-union. The best outcomes were achieved with 2000 impulses at 0.2 mJ/mm2 in 2 sessions. For non-union, there are individual randomised, controlled studies as well as case series. The healing rates with shock wave therapy do not differ from those following surgery. In the studies 4000 impulses were applied at an energy flow density of 0.09 – 0.7 mJ/mm2 in each of generally 3 or 4 sessions.
Pulsating electromagnetic field therapy (PEMF)
PEMF is another procedure being advocated for non-union and delayed healing. Studies have demonstrated good healing of Jones fractures with non-union, particularly when the devices have been used for more than 9 hours a day [24]. Fracture healing was more quickly achieved following surgery in the treatment group than in the group receiving placebo magnetic field therapy [34]. The evidence of the results, however, is problematic because a control group was part of the study design in only one of the studies.
Ultrasound
Studies point to improved healing in non-union, but in some there was no control group [35, 14]. Good healing rates were achieved, and individual studies indicate greater cost effectiveness compared with surgical revision [14].
Platelet rich plasma (PRP)
Animal studies have shown positive effects of PRP on fracture healing [13]. In view of these results a beneficial effect is also conceivable in humans. Clinical experience shows that additional treatment with PRP does lead to a positive course in a protracted course of fracture healing. Overall, the evidence for PRP promoting fracture healing is scarce [29]. On the other hand, injection of PRP has been successful in alleviating pain and in associated biomechanical compensation mechanisms as well as protective guarding and movement avoidance [25, 37]. However, further evidence-based studies are required for a more evidence-based and conclusive assessment [16].
Summary
The first important step in the treatment of metatarsal stress fractures is to figure out the cause and identify any risk factors. It can help prevent secondary injury. This should be followed by multimodal treatment comprising modified weight bearing and optimised bone healing. The pain experienced by the patient plays a central role particularly with regard to modifying weight bearing. However, due to their negative effect on fracture healing, administration of NSAIDs should be avoided. Pain can be reduced, and bone healing promoted by diet, shock wave therapy and, when applicable, supplementary electromagnetic field therapy.
Autoren
ist wissenschaftliche Koordinatorin am LANS Medicum. Sie hat sich zuvor an der Deutschen Sporthochschule Köln in Exercise Science and Coaching (M. Sc.) spezialisiert und war selbst im Schwimmleistungssport aktiv.
ist Facharzt für Orthopädie und Unfallchirurgie, Spezielle Unfallchirurgie und Sportmedizin. Er ist Gründer und Inhaber des LANS Medicum. Seine mannschaftsärztlichen Betreuungen umfassten u. a. das Handballteam des HSV sowie von 2011-2014 die Erstligafußballmannschaft des Hamburger SV. Heute betreut er mit seinem Team mehrere Fußball- und Hockeyteams sowie das Hamburger Ballett von John Neumeier. Außerdem ist Prof. Catalá-Lehnen als Professor für den Schwerpunkt Orthopädie an der Medical School Hamburg und am UKE in der Lehre für das Fach Knochenpathologie tätig.
ist Sportwissenschaftler und Assistenzarzt in der Weiterbildung zum Facharzt für Orthopädie und Unfallchirurgie am Städtischen Klinikum Lüneburg. Am LANS Medicum betreut er die Leistensprechstunde.