The prevalence of osteoarthritis is increasing, necessitating further development and optimization of conservative, multimodal therapy concepts. In this context, hyaluronic acid (HA) products have become established in everyday orthopedic practice and sports medicine. Despite ongoing debates on the effectiveness of intra-articularly administered HA (IA-HA), the market for viscosupplements (VS) is steadily growing. In 2021, the market was valued at $ 4.4 billion, with a forecasted growth to $ 10.9 billion by 2031, underscoring the increasing demand and potential in this field [1). New combinations of active ingredients and product innovations are driving market and result in numerous scientific publications [2].
Prevalence of osteoarthritis
In 2020, approximately 595 million people worldwide – about 7.6 % of the total population – were affected by osteoarthritis. A forecast published in the Lancet (2023) estimates that if current trends continue, around 1 trillion people worldwide could be affected by osteoarthritis by 2050 [3] due to demographic change [4].
The knee is the most affected joint. The age-standardized prevalence of knee osteoarthritis (KOA) in 2020 was around 4,307 cases per 100,000 people worldwide. Symptomatic KOA often leads to severe pain, limited mobility and significant limitations in quality of life due to reduced independence in everyday activities [5, 6].
Given the high socio-economic burden of musculoskeletal diseases, the World Health Organization (WHO) launched the Bone and Joint Decade to improve research and address the growing challenges in the healthcare system [4].
Currently, the treatment of OA primarily focuses on symptom control. The development of disease-modifying osteoarthritis drugs is complicated by factors such as the complexity of the disease and the heterogeneity of patient populations. Nevertheless, promising results are being observed in clinical trials involving new combinations of active ingredients targeting cartilage repair, cellular senescence, and homeostasis [7].
Current recommendations
The efficacy of IA-HA remains controversial in scientific literature and requires a differentiated consideration of the existing evidence. International clinical guidelines differ considerably regarding the recommendations for IA-HA use in KOA [8].
A recent review of ‚current clinical practice guidelines‘ indicates that IA-HA is widely part of the treatment management of KOA in global guidelines [9].
Based on the results of a ‚Delphi consensus process‘, an expert panel of the EUROVISCO group published consensus guidelines for IA-HA in KOA in 2024. The resulting 34 statements include for instance strong recommendations for IA-HA injections [10], can serving as a valuable resource for clinicians deve-loping individualized treatment algorithms.
The German Society for Orthopedics and Trauma Surgery (DGOU) is expected to publish the S3 guideline “Prevention and treatment of osteoarthritis of the knee” shortly. Until then, the recommendations will continue to be based on the S2k guideline ‘Osteoarthritis of the knee’, which makes the open recommendation “can be considered” for IA-HA.
When selecting a VS, the cost-effectiveness of hyaluronic acid products should also be taken into account, considering factors like biochemical composition, combinations of active ingredients, and different patient populations [2].
Regarding pain outcomes, a network meta-analysis following IA-HA application indicated a minimal clinically important difference (MCID) and an effect size of 0.34 – 0.63 (modest / moderate effects), showing better results than in control groups treated with corticosteroids and paracetamol [11]. However, other systematic evidence suggests only a slight reduction in pain following IA-HA treatment, leading to concerns about clinical significance [12]. Short-term pain relief after IA-HA was shown in a systematic review of RCTs published in 2024 [13]. A literature analysis from 2024 presents varying data on effect sizes and describes indications of publication bias [14]. Given these findings, clinical relevance should be critically assessed and treatment recommendations individually discussed with the patients.
Properties of HYALURONIC ACID and predictors of response
To enhance the effectiveness of IA-HA injections, it is important to consider several predictors of response, including the stage of disease, age, body mass index, comorbidities and radiological findings [10].
Product Overview
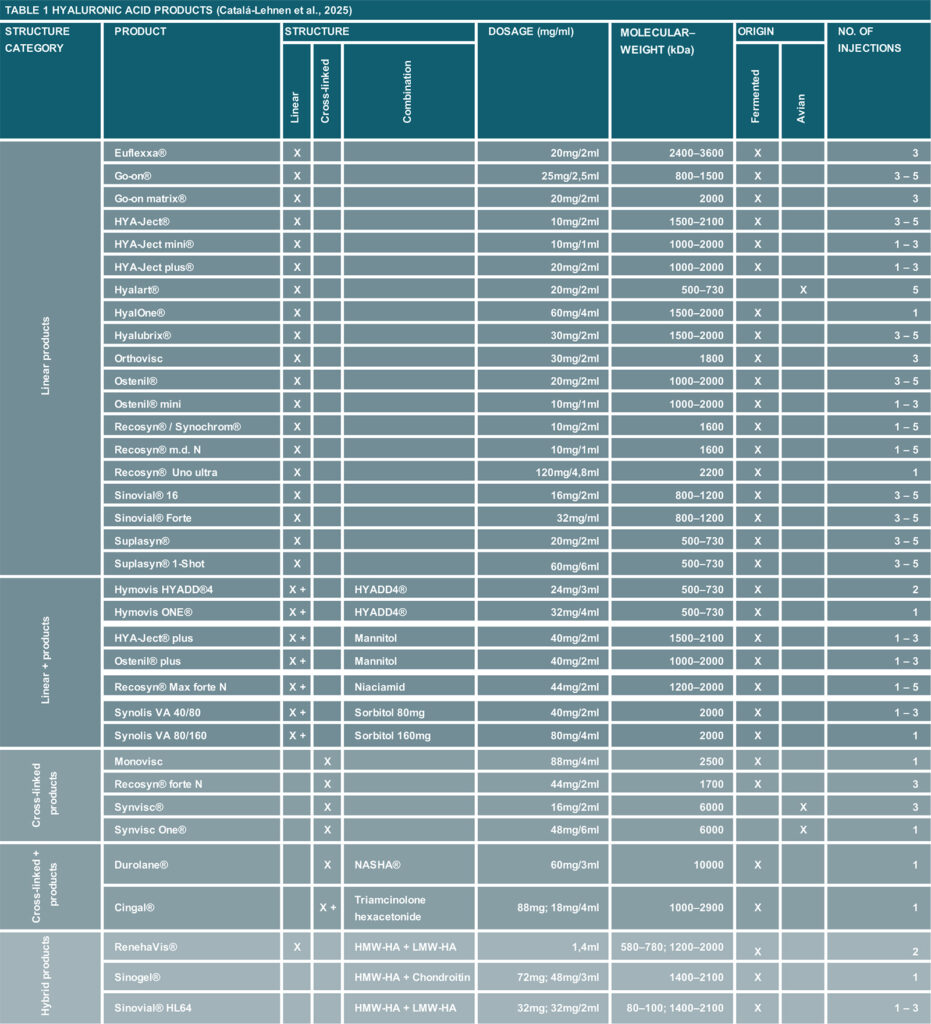
Table 1 provides an overview of different HA products (based on the manufacturer’s specifications) for IA use, specifically used in sports medicine to help healthcare professionals select the most appropriate product.
The products are categorized based on their structure and formulation, which includes linear HA, cross-linked HA, and combination types. Each product is categorized by its dosage (mg / ml) in kDa, reflecting the molecular weight of the HA. The origin of the HA is noted, distinguishing between fermented and avian sources, influencing the product’s properties and suitability for different treatments and populations (e. g., regarding intolerances).
Given HA’s slow-release properties, it is recommended to combine it with supportive components or agents. Currently available combination products can be found in Table 1 (Structure – Combination).
Summary
IA-HA is an important component of a multimodal approach to OA management [10]. When selecting a product for IA injection, it is crucial to recognize the differences among available products. Further development and optimization of treatment algorithms incorporating orthobiological therapy options (such as PRP, collagen, ACS) are necessary to ensure safe and efficient patient treatment. The following goals should be focused on to advance treatment algorithms in sports medicine:
- Improvement of clinical outcomes.
- Improvement of clinical efficacy through innovative combinations of DMOADs active ingredients – product developments.
- Optimization of the indication-specific use of HA preparations (differences in active ingredient combinations…) in orthobiological treatment algorithms.
- Review of the necessity for research to address current study limitations and to avoid “research waste”.
Literature
- Allied Market Research. Viscosupplementation market research, 2031. Verfügbar unter: https://www.alliedmarketresearch.com/viscosupplementation-market.
- Ferkel E, Manjoo A, Martins D, Bhandari M, Sethi P, Nicholls M. Intra-articular Hyaluronic Acid Treatments for Knee Osteoarthritis: A Systematic Review of Product Properties. Cartilage. Dezember 2023;14(4):424–32.
- Steinmetz JD, Culbreth GT, Haile LM, Rafferty Q, Lo J, Fukutaki KG, u. a. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 1. September 2023;5(9):e508–22.
- Fuchs J, Kuhnert R, Scheidt-Nave C. 12-Monats-Prävalenz von Arthrose in Deutschland. 2. Aufl. 2017; Verfügbar unter: DOI 10.17886/RKI-GBE-2017-054
- Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J. Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol Orthop Traumatol. Mai 2019;29(4):947–55.
- D’Ambrosi R, Mangiavini L, Loucas R, Loucas M, Brivio A, Mariani I, u. a. Similar rate of return to sports activity between posterior-stabilised and cruciate-retaining primary total knee arthroplasty in young and active patient. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. Februar 2023;31(2):551–8.
- Zhao Y, Ou Q, Cai Y, Ruan G, Zhang Y, Ding C. Shedding light on experimental intra-articular drugs for treating knee osteoarthritis. Expert Opin Investig Drugs. Juni 2023;32(6):509–24.
- Overton C, Nelson AE, Neogi T. Osteoarthritis Treatment Guidelines from Six Professional Societies: Similarities and Differences. Rheum Dis Clin North Am. August 2022;48(3):637–57.
- Phillips M, Bhandari M, Grant J, Bedi A, Trojian T, Johnson A, u. a. A Systematic Review of Current Clinical Practice Guidelines on Intra-articular Hyaluronic Acid, Corticosteroid, and Platelet-Rich Plasma Injection for Knee Osteoarthritis: An International Perspective. Orthop J Sports Med. 1. August 2021;9(8):23259671211030272.
- Conrozier T, Raman R, Diraçoglu D, Montfort J, Bard H, Baron D, u. a. EUROVISCO Consensus Guidelines for the Use of Hyaluronic Acid Viscosupplementation in Knee Osteoarthritis Based on Patient Characteristics. Cartilage. 20. November 2024;19476035241271970.
- Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, McAlindon TE. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 6. Januar 2015;162(1):46–54.
- Pereira TV, Jüni P, Saadat P, Xing D, Yao L, Bobos P, u. a. Viscosupplementation for knee osteoarthritis: systematic review and meta-analysis. BMJ. 6. Juli 2022;378:e069722.
- Migliorini F, Maffulli N, Schäfer L, Kubach J, Betsch M, Pasurka M. Less Pain with Intra-Articular Hyaluronic Acid Injections for Knee Osteoarthritis Compared to Placebo: A Systematic Review and Meta-Analysis of RandomisedControlled Trials. Pharm Basel Switz. 20. November 2024;17(11).
- Büchter R, Pieper D. Hyaluronsäure bei Kniearthrose – Sinvolle IGeL oder Placebo? Netzw Evidenzbasierte Med. 2024;(06).
- Passi A, Vigetti D. Hyaluronan as tunable drug delivery system. Adv Drug Deliv Rev. Juni 2019;146:83–96.
Autoren
ist Facharzt für Orthopädie und Unfallchirurgie, Spezielle Unfallchirurgie und Sportmedizin. Er ist Gründer und Inhaber des LANS Medicum. Seine mannschaftsärztlichen Betreuungen umfassten u. a. das Handballteam des HSV sowie von 2011-2014 die Erstligafußballmannschaft des Hamburger SV. Heute betreut er mit seinem Team mehrere Fußball- und Hockeyteams sowie das Hamburger Ballett von John Neumeier. Außerdem ist Prof. Catalá-Lehnen als Professor für den Schwerpunkt Orthopädie an der Medical School Hamburg und am UKE in der Lehre für das Fach Knochenpathologie tätig.
ist Sportphysiotherapeutin und GCP-zertifizierte (AMG und MPDG) Studienkoordinatorin. Sie ist Head of Science am LANS Medicum Hamburg, studierte in Hamburg und Plymouth (UK) und schloss mit einem MSc Advanced Professional Practice in Physiotherapy mit dem Schwerpunkt Clinical Research ab.
Studium der Humanmedizin an der LMU München, Bern und VR China. Facharzt für Neurologie, spezielle Schmerztherapie und Rehabilitationswesen, Dozent und Ausbilder für Ärzte in der Schmerztherapie. Medizinischer Direktor für diverse Firmen.
© Andreas Kuhrau





