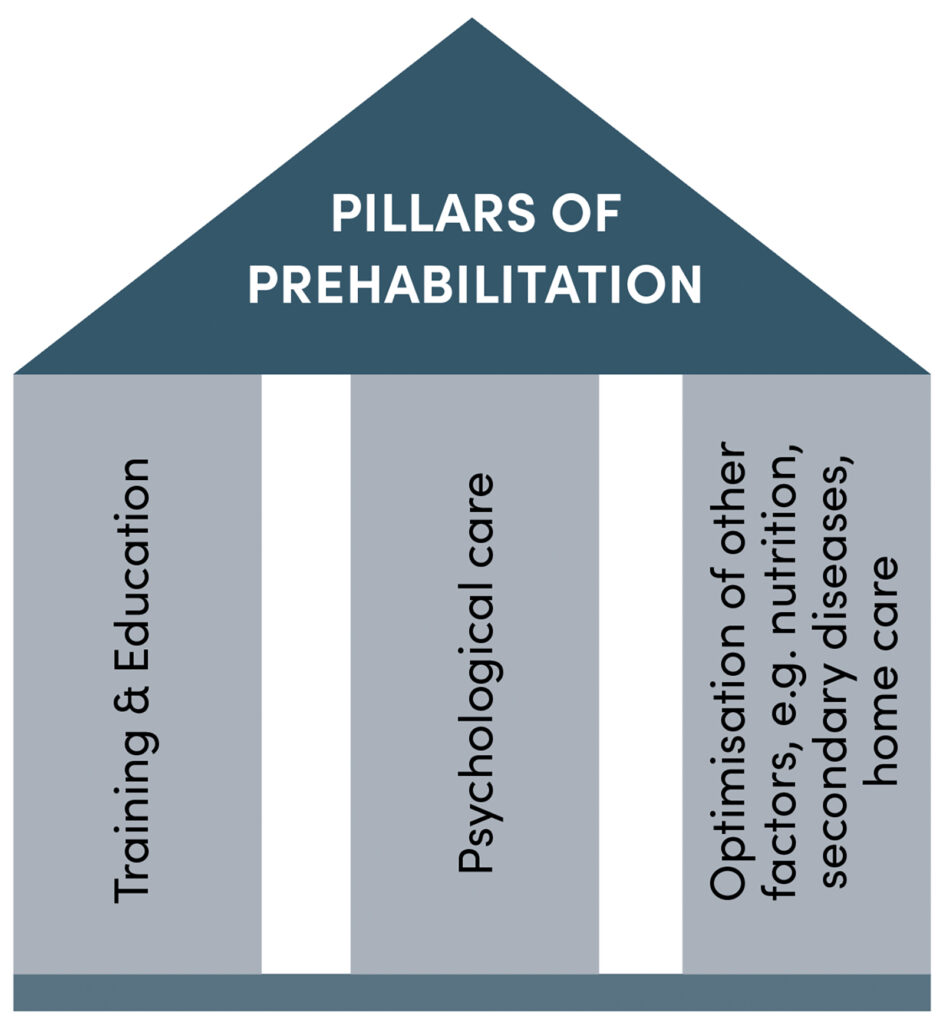
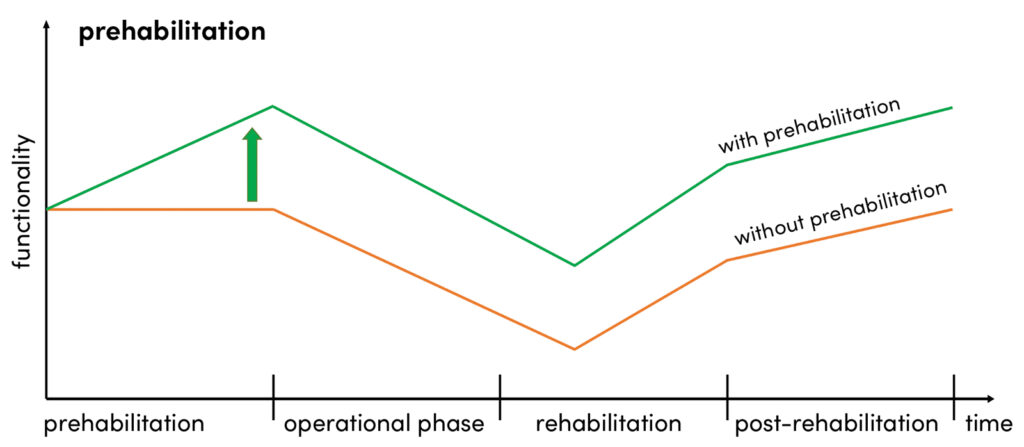
Prehabilitation is becoming increasingly important in the rehabilitation of orthopaedic injuries. It involves targeted physical, psychological and socio-medical preparation to promote rapid and full recovery. In addition to special training, it includes the optimisation of risk factors such as secondary diseases, nutrition, socio-medical planning and psychological preparation.
A frequently cited argument against prehabilitation is the delay in surgical treatment of a fresh ACL injury. However, studies show that delayed reconstruction, compared to early reconstruction, has no negative effects on secondary knee pathologies or self-assessed knee function after two years [8]. Instead, delaying the reconstruction allows for the identification of compensatory mechanisms and the targeted promotion of the patient’s functional abilities preoperatively [9].
Phases of prehabilitation
Prehabilitation can be divided into two phases: Phase 1 aims to restore the knee to homeostasis by reducing inflammation, pain and swelling [7, 11]. After about two weeks, phase 2 begins, in which muscle strength and neuromuscular control are to be restored or maintained [11]. Training should include exercises to strengthen the lower extremity, with a focus on knee joint extensors and flexors, neuromuscular training, stretching, and ROM exercises [3, 5]. Single-leg jumps and perturbation training can also be incorporated [10]. Although specific evidence-based guidelines for the early phase are lacking, protocols from Eitzen and Wilk provide orientation [5, 7, 11]. The intensity of the exercises depends on the patient’s pre-traumatic performance, training options, compliance and the condition of the knee. The literature recommends training 2 – 4 times a week for 75 – 120 minutes, including a 10 – 20 minute warm-up [4, 12–15].
Phase 1: Improvement range of motion, pain and swelling reduction
The most common complication after ACLR is loss of mobility, especially in full knee extension, leading to abnormal joint arthrokinematics and increased patellofemoral/tibiofemoral pressure [16 – 19]. To improve extension and flexion, passive and active ROM exercises with the help of elastic bands are helpful [15, 19]. Mobility exercises should be held for at least 30 seconds and performed several times a day. Wilk et al. recommend 60 minutes of daily stretching time at low intensity [7]. Immediately after the injury, the focus is on reducing swelling and pain [20]. Pain can inhibit muscle activity and impair quadriceps function. Preoperative cooling improves the postoperative pain situation in the short term and reduces the need for medication [21]. As part of the trend towards more outpatient treatment, cruciate ligament surgery requires a standardised procedure that also includes preoperative optimisation and pain management. Enhanced recovery programmes play a central role here.
Phase 2: progressive strength training
Targeted exercises as part of prehabilitation can improve functional and muscular performance as well as lower limb symmetry index (LSI) six months postoperatively compared to patients without prehabilitation [1 – 3]. Studies also show positive effects on return to sport (RTS) and subjectively perceived knee function up to two years after reconstruction [4, 5]. Progressive strength training is a central component of prehabilitation. Eitzen et al. showed that preoperative quadriceps strength is a crucial predictor of knee function two years after ACL reconstruction, although preoperative deficits can persist in the long term [25]. In addition to maintaining the trunk and leg muscles, the focus is on improving muscular control. Patients who had undergone preoperative training showed less loss of extension strength postoperatively [15], while hamstring peak torque increased in both groups [14]. Both open- and closed-kinetic-chain exercises and concentric, eccentric, and isometric strength exercises are suitable. Open-chain exercises significantly improve quadriceps strength and are less problematic in terms of anterior translation than previously assumed [27, 28]. A progressive training programme, for example, involves 3 – 4 sets of 6 – 8 repetitions and a gradual increase in load according to the ‘+2’ principle [4, 12, 25]. Alternatively, a weekly increase in load of 10–15 % can be applied [14].
Plyometrics, balance and perturbation training
Single-leg jumping tests, in particular the Single Leg Hop for Distance (SDH), are reliable tools for assessing the rehabilitation process and knee joint stability in ACL injuries and after reconstructions [30].
The SDH combines leg strength and neuromuscular control and reflects the confidence of patients in the injured /operated knee. It also allows conclusions to be drawn about the resilience of sport-specific requirements and, in combination with quadriceps strength, has a predictive significance for recurrent ACL injuries [31]. Prehabilitation can improve SDH performance of the injured limb by 13.5 % compared to 9 % in a control group. At 12 weeks post-surgery, the prehabilitation group showed significantly less loss of performance in SDH [14]. In addition to the SDH, recommended exercises include stepper hops with a soft landing and controlled lateral jumps (3 – 5 repetitions) [11, 14, 15, 19].
Eitzen et al. recommend plyometric exercises that emphasise soft landings in the knee-over-toe position to avoid harmful stresses [11]. The Sideways Single-Leg Hop is recommended in 3 sets of 15 jumps, while the Stepper Hop can be incorporated as a single set of 15 repetitions [11]. Balance training can be incorporated early in prehabilitation. Studies have shown significant improvements in balance exercises, both with eyes open and closed, in the prehabilitation group [19]. This can include, for example, single-leg squats and standing on balance pads or boards [11, 19]. Standing on one leg is recommended for 30 seconds to 3 minutes with eyes open and 5 – 10 seconds with eyes closed. For single-leg squats on balance pads, 2 sets of 20 repetitions are suitable, depending on the quality of execution [11].
Perturbation training requires a largely restored control of the quadriceps and hamstring muscles and should be increased gradually over several weeks [11]. Patients who completed a prehabilitation programme consisting of neuromuscular training, strength training and perturbation training showed better functional results and higher RTS rates than the control group two years after ACL reconstruction. In addition, the rate of giving-way events in ACL insufficiency was reduced [4, 11]. The training includes, among other things, single- and two-legged standing exercises on rolling or rocking boards in anterior-posterior or medial-lateral alignment. To increase the difficulty, diagonal movements, rotations, arm movements and self-initiated perturbations were integrated. In later phases, exercises with balls were added, such as throwing, catching or blocking [11, 19]. Neuromuscular training combines plyometric training, balance training and perturbation training. Studies show improvements in mobility and balance in training groups. Exercises should be performed at the end of the session to promote neuromuscular control under fatigue [7, 29].
Important: Despite the recommendations and guidelines given, prehabilitation training should always be adapted to the specific needs and abilities of each patient.
„Innovative surgical sciences 4.4 (2019): 132-138. © Dr. med. Robert Percy Marshall (adapted)
Addressing other risk factors as part of prehabilitation:
Nutrition
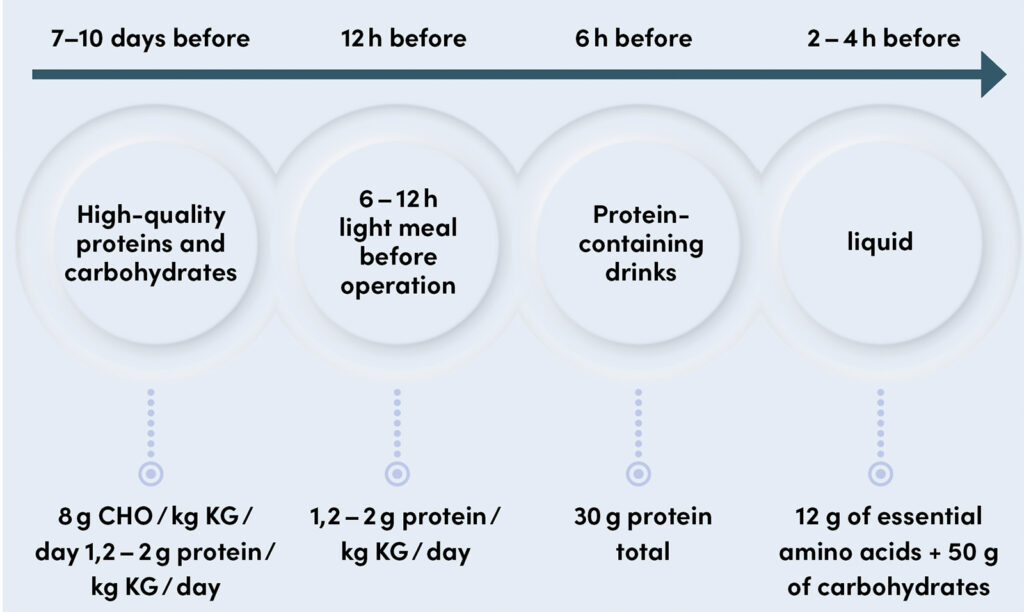
The nutritional status of the patient before and after surgery is a crucial factor for the outcome of musculoskeletal diseases. A high-protein, high-carbohydrate diet is recommended 7 – 10 days before surgery to promote wound healing, graft healing, and to prevent muscular atrophy [33, 34]. The increased caloric requirement due to the injury (20 % – 100 % more) requires a caloric balance, whereby both over- and undersupply must be avoided. A minimum intake of 2.0 g / kg body weight of amino acids (e.g., lysine, leucine, glutamine, arginine) is recommended [35]. Micronutrients such as zinc, boron, selenium and silicon play a central role in wound healing [34, 36]. In addition, creatine monohydrate, omega-3 fatty acids and vitamins C, D3 and E can be useful, as established in competitive sports [34, 37]. However, comprehensive RCT studies that clearly demonstrate their effectiveness are still lacking [39].
Sports psychology and education
Good physiological results after a sports injury do not always correlate with long-term satisfaction or quality of life [40]. Psychological processing plays an important role in regeneration after ACL injuries. Psychological factors that influence recovery should be identified as early as the prehabilitation phase [41]. Self-assessment is a central indicator of the physical and psychological state of the patient [12]. For physically active, mostly younger patients, an ACL injury often represents an unexpected burden, particularly due to high expectations of recovery and return to performance, especially in professional athletes. Many patients find it difficult to assess their actual leg axis stability and resilience, which often leads to over- or underestimation [43]. This insecurity, combined with the fear of re-injury and the pressure to return quickly, increases the psychological burden [41, 42, 44]. The data on education and compliance in prehabilitation for ACL injuries and their influence on the treatment outcome is limited. However, self-confidence, optimism and self-motivation certainly have a positive influence on the outcome and compliance and should be encouraged during prehabilitation [44]. Despite optimal training planning, psychological support, patient education and optimisation of the preoperative setting, external factors such as training opportunities, professional and family situation influence the outcome of an ACL injury and require special attention.
Conclusion
Prehabilitation after ACL injury lays the foundation for an optimal postoperative outcome. It includes not only basic measures and targeted training, but also the addressing of further risk factors such as education, psychological support, nutrition and pain management in order to create the best possible conditions for a successful operation and rehabilitation. The planning and implementation of prehabilitation must be individually coordinated with patients, therapists and cost units. In the future, the focus should be on creating structured, quality-assured concepts for prehabilitation in order to enable patients to prepare for the surgical and postoperative phase in an evidence-based and effective way.
This article is a highly abbreviated of the article published in 2023 Valle, C., Marshall, R. C., & Mengis, N. (2023). Prehabilitation for anterior cruciate ligament injuries. Knee Journal, 5(1), 3–11. https://doi.org/10.1007/s43205-022-00188-2
Bibliography
1. Logerstedt, D., et al., Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction.Knee Surg Sports Traumatol Arthrosc, 2013. 21(4): p. 859-68.
2. Alshewaier, S., G. Yeowell, and F. Fatoye, The effectiveness of pre-operative exercise physiotherapy rehabilitation on the outcomes of treatment following anterior cruciate ligament injury: a systematic review. Clin Rehabil, 2017. 31(1): p. 34-44.
3. Hartigan, E., M.J. Axe, and L. Snyder-Mackler, Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res, 2009. 27(6): p. 724-9.
4. Failla, M.J., et al., Does Extended Preoperative Rehabilitation Influence Outcomes 2 Years After ACL Reconstruction? A Comparative Effectiveness Study Between the MOON and Delaware-Oslo ACL Cohorts. Am J Sports Med, 2016. 44(10): p. 2608-2614.
5. Giesche, F., et al., Evidence for the effects of prehabilitation before ACL-reconstruction on return to sport-related and self-reported knee function: A systematic review. PLoS One, 2020. 15(10): p. e0240192.
6. Lepley, L.K. and R.M. Palmieri-Smith, Pre-operative quadriceps activation is related to post-operative activation, not strength, in patients post-ACL reconstruction. Knee Surg Sports Traumatol Arthrosc, 2016. 24(1): p. 236-46.
7. Kevin E. Wilk, C.A.A., Preoperative Phase in the Rehabilitation of the Patient Undergoing Anterior Cruciate Ligament Reconstruction. Operative Techniques in Sports Medicine, 2016. 24(1): p. 12-20.
8. Frobell, R.B., et al., A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med, 2010. 363(4): p. 331-42.
9. Kaplan, Y., Identifying individuals with an anterior cruciate ligament-deficient knee as copers and noncopers: a narrative literature review. J Orthop Sports Phys Ther, 2011. 41(10): p. 758-66.
10. van Melick, N., et al., Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med, 2016. 50(24): p. 1506-1515.
11. Eitzen, I., et al., A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther, 2010. 40(11): p. 705-21.
12. Grindem, H., et al., How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med, 2015. 49(6): p. 385-9.
13. Zdunski, S., et al., Evaluation of the Effectiveness of Preoperative Physiotherapy Using the Lysholm-Gillquist Scale in Patients Qualified for Surgical Arthroscopic Anterior Cruciate Ligament Reconstruction – Pilot Study. Ortop Traumatol Rehabil, 2015. 17(3): p. 249-58.
14. Shaarani, S.R., et al., Effect of prehabilitation on the outcome of anterior cruciate ligament reconstruction. Am J Sports Med, 2013. 41(9): p. 2117-27.
15. Kim, D.K., J.H. Hwang, and W.H. Park, Effects of 4 weeks preoperative exercise on knee extensor strength after anterior cruciate ligament reconstruction. J Phys Ther Sci, 2015. 27(9): p. 2693-6.
16. Austin, J.C., C. Phornphutkul, and E.M. Wojtys, Loss of knee extension after anterior cruciate ligament reconstruction: effects of knee position and graft tensioning. J Bone Joint Surg Am, 2007. 89(7): p. 1565-74.
17. Harner, C.D., et al., Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med, 1992. 20(5): p. 499-506.
18. Rubin, L.E., P.C. Yeh, and M.J. Medvecky, Extension loss secondary to femoral-sided inverted cyclops lesion after anterior cruciate ligament reconstruction. J Knee Surg, 2009. 22(4): p. 360-3.
19. Keays, S.L., et al., The effectiveness of a pre-operative home-based physiotherapy programme for chronic anterior cruciate ligament deficiency. Physiother Res Int, 2006. 11(4): p. 204-18.
20. C.H., B., Blowing out your knee: ACL tear and pain management. U.S. Pharmacist, 2011. 36.
21. Koyonos, L., et al., Preoperative cryotherapy use in anterior cruciate ligament reconstruction. J Knee Surg, 2014. 27(6): p. 479-84.
22. Kavak Akelma, F., et al., The effects of pregabalin and adductor canal block on postoperative pain in arthroscopic anterior cruciate ligament reconstruction. Turk J Med Sci, 2020. 50(1): p. 195-204.
23. Beck, P.R., et al., Postoperative pain management after anterior cruciate ligament reconstruction. J Knee Surg, 2004. 17(1): p. 18-23.
24. Cina-Tschumi, B., [Evidence-based impact of cryotherapy on postoperative pain, swelling, drainage and tolerance after orthopedic surgery]. Pflege, 2007. 20(5): p. 258-67.
25. Eitzen, I., I. Holm, and M.A. Risberg, Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med, 2009. 43(5): p. 371-6.
26. Kraemer, W.A., K.; Cafarelli, E, American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc, 2009. 41(3): p. 687-708.
27. Tagesson, S., et al., A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: a randomized clinical trial evaluating dynamic tibial translation and muscle function. Am J Sports Med, 2008. 36(2): p. 298-307.
28. Morrissey, M.C., M.C. Perry, and J.B. King, Is knee laxity change after ACL injury and surgery related to open kinetic chain knee extensor training load? Am J Phys Med Rehabil, 2009. 88(5): p. 369-75.
29. Lattanzio, P.J. and R.J. Petrella, Knee proprioception: a review of mechanisms, measurements, and implications of muscular fatigue. Orthopedics, 1998. 21(4): p. 463-70; discussion 470-1; passim.
30. Reid, A., et al., Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther, 2007. 87(3): p. 337-49.
31. Ashigbi, E.Y.K., W. Banzer, and D. Niederer, Return to Sport Tests‘ Prognostic Value for Reinjury Risk after Anterior Cruciate Ligament Reconstruction: A Systematic Review. Med Sci Sports Exerc, 2020. 52(6): p. 1263-1271.
32. Quack, V., et al., [Multidisciplinary Rehabilitation and Fast-track Rehabilitation after Knee Replacement: Faster, Better, Cheaper? A Survey and Systematic Review of Literature]. Rehabilitation (Stuttg), 2015. 54(4): p. 245-51.
33. Hirsch, K.R., R.R. Wolfe, and A.A. Ferrando, Pre- and Post-Surgical Nutrition for Preservation of Muscle Mass, Strength, and Functionality Following Orthopedic Surgery. Nutrients, 2021. 13(5).
34. Smith-Ryan, A.E., et al., Nutritional Considerations and Strategies to Facilitate Injury Recovery and Rehabilitation. J Athl Train, 2020. 55(9): p. 918-930.
35. Papadopoulou, S.K., Rehabilitation Nutrition for Injury Recovery of Athletes: The Role of Macronutrient Intake. Nutrients, 2020. 12(8).
36. Shaw, G., B. Serpell, and K. Baar, Rehabilitation and nutrition protocols for optimising return to play from traditional ACL reconstruction in elite rugby union players: A case study. J Sports Sci, 2019. 37(15): p. 1794-1803.
37. Owens, D.J., et al., Exercise-induced muscle damage: What is it, what causes it and what are the nutritional solutions? Eur J Sport Sci, 2019. 19(1): p. 71-85.
38. Wall, B.T., J.P. Morton, and L.J. van Loon, Strategies to maintain skeletal muscle mass in the injured athlete: nutritional considerations and exercise mimetics. Eur J Sport Sci, 2015. 15(1): p. 53-62.
39. Greif, D.N., et al., Supplement Use in Patients Undergoing Anterior Cruciate Ligament Reconstruction: A Systematic Review.Arthroscopy, 2020. 36(9): p. 2537-2549.
40. Truong, L.K., et al., Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br J Sports Med, 2020. 54(19): p. 1149-1156.
41. Khalladi, K., et al., Sleep and psychological factors are associated with meeting discharge criteria to return to sport following ACL reconstruction in athletes. Biol Sport, 2021. 38(3): p. 305-313.
42. Padaki, A.S., et al., Prevalence of Posttraumatic Stress Disorder Symptoms Among Young Athletes After Anterior Cruciate Ligament Rupture. Orthop J Sports Med, 2018. 6(7): p. 2325967118787159.
43. Fitzgerald, G.K., M.J. Axe, and L. Snyder-Mackler, A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc, 2000. 8(2): p. 76-82.
44. Everhart, J.S., T.M. Best, and D.C. Flanigan, Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc, 2015. 23(3): p. 752-62.
45. Thoma, L.M., et al., Coper Classification Early After Anterior Cruciate Ligament Rupture Changes With Progressive Neuromuscular and Strength Training and Is Associated With 2-Year Success: The Delaware-Oslo ACL Cohort Study. Am J Sports Med, 2019. 47(4): p. 807-814.
Autoren
ist Fachärztin für Physikalische und Rehabilitative Medizin. Sie ist als Oberärztin in der Rehabilitationsklinik Medical Park Chiemsee Schwerpunkt Orthopädie und Sportorthopädie und als wissenschaftliche Mitarbeiterin in der Klinik und Poliklinik für Orthopädie und Sportorthopädie am Klinikum rechts der Isar mit dem Forschungsschwerpunkt „Wearables and AI in Orthopaedics“ tätig. Sie ist neben anderen nationalen und internationalen Fachgesellschaften Mitglied des Komitees für Prävention, Rehabilitation und konservative Therapie der Deutschen Kniegesellschaft (DKG) und im Vorstand der DKG als Beirat tätig.
ist Facharzt für Physikalische und Rehabilitative Medizin und seit 2025 beim AFC Bournemouth als Director of Medical and Performance tätig. Davor war ab 2018 Mannschaftsarzt von RB Leipzig. Als Gründungsmitglied des Athleticums am Universitätskrankenhaus Hamburg-Eppendorf ab 2012 für die medizinische Betreuung des HSV, zunächst für das komplette NLZ, von 2014 – 2017 auch stellvertretend für die Bundesligamannschaft zuständig. Spezialgebiete: konservative Orthopädie, alternative Heilmethoden, Mikronährstofftherapie. Außerdem ist er wiss. Beirat der sportärztezeitung.
ist Fachärztin für Orthopädie und Unfallchirurgie mit der Zusatzbezeichnung Sportmedizin. Sie ist als Oberärztin am Universitären Zentrum Bewegungsapparat des Kantonsspital Baselland tätig, zertifizierte DKG Kniechirurgin und AGA Faculty Member. Als Mitglied des Komitees Ligamentverletzungen der Deutschen Kniegesellschaft war sie maßgeblich an der Entwicklung der Return to Sport Testmanuale beteiligt.