An increasing number of publications within the last few years highlights the growing interest in Orthobiologics and its status in sports medicine, especially for the therapy of overuse-related and regenerative damage (see article by Dr. Dr. Andreas Först „Orthobiologika“ in sportärztezeitung 1/24) (4).
Orthobiologics currently available for typical orthopaedic pathologies include hyaluronic acid (HA), platelet-rich plasma (PRP), autologous conditioned serum (ACS), bone marrow aspirate concentrate (BMAC), bone marrow-derived stem cells (BMSCs), adipose-derived mesenchymal stem cells (AD-MSCs) and synthetic scaffolds, besides others for trauma surgery (5).
With a worldwide prevalence of 22.9% (>40-year-olds) (6) and effects on the quality of life and activities of daily living of those affected, knee osteoarthritis (KOA) leads to considerable social consequences and economic costs (7). Consequently, new preventive and conservative therapy options and treatment approaches, especially in sports medicine, will continue to be of great importance. The advantages of Orthobiologics are their therapeutic potential, minimal invasiveness, and ‚manageable‘ costs compared to surgical therapies (8).
Clinical Guideline Recommendations
The S2k-Gonarthrosis Living Guideline of the German Society for Orthopaedics and Trauma Surgery recommends strength, endurance and mobility training as part of the conservative treatment of KOA. According to the recommendation updated in 2023, intra-articular corticosteroids injections as short-term management can be considered for treating painful KOA if the dose is as low as possible but effective and the application follows clinical guidelines (9).
However, corticosteroid injections should be carefully considered given the current evidence of significant side effects such as inhibition of cartilage metabolism and possible reduction of cartilage mass (see article by Prof. Dr. Götz Welsch „Update Intraartikuläre Injektionen: Eine aktuelle Literatur-Übersicht“ in sportärztezeitung 4/23) (10–12).
Side effects can be classified either into local or systemic and immediate or delayed effects, which may depend on the target group (e.g., athletes) and should, therefore, be individually considered (13).
Intra-articular HA injections may be considered in patients in whom the use of NSAIDs is contraindicated or not sufficiently effective. No recommendation can currently be made for a specific PRP preparation/development process (9).
The application of collagen in various diseases of the musculoskeletal system is being discussed increasingly. The first positive outcomes have already been reported for example in patients with KOA (14-19).
In a recent RCT, hydrolyzed collagen peptides led to pain relief and improved functional status and quality of life in patients with collateral ligament pain of the knee compared to the control group receiving oral pain medication and corticosteroid injection, without reported intergroup differences. The intervention group reported higher satisfaction compared to the control group, and no adverse events were documented. Thus, collagen may be a promising treatment alternative and/or adjunct, potentially circumventing the side effects of corticosteroid injections (20).
Collagen
Collagen is a fundamental structural element of connective tissue (organic: bones, teeth, cartilage, tendons, ligaments) and makes up >30% of the total protein in humans (21-23). A total of 28 different types of collagens are distinguished, some of whose functions are still unclear (24):
- Collagen type I – fibre-forming in collagen fibres: skin, tendons, bone, dentin, fibrocartilage, cornea
- Collagen type II – fibre-forming: hyaline and elastic cartilage, vitreous body
- Collagen type III – fibre-forming in reticulin fibres: skin, skeletal muscles, blood vessels
Collagen is structurally composed of three long, left-handed amino acid chains (two identical α-1 chains and one α-2 chain) coiled into a compact right-handed triple helix (25). Enzymatic hydrolysis breaks collagen into smaller peptides, affecting bioavailability and absorption in the body. Due to the molecular weight of <3,000 Daltons, collagen peptides have a high biocompatibility (26,27). The mode of action of collagen is based on complex mechanisms that have not yet been understood in detail and require further clinical testing (15).
Cautious positive findings indicate a possible benefit of oral collagen supplementation (type II native or hydrolysate) for osteoarthritis (see article by Prof. Dr. Nadine Berling und Ronny Heldt-Döpel „Kollagene im Sport: Arthroseprävention und -therapie“ in der sportärztezeitung 3/23) (26). Collagen supplementation has provided initial evidence of increased mineral mass and bone density and inhibition of inflammatory cytokines in animal and human studies (28).
In their review, Lin et al. (2023) found a significant reduction in pain in patients with KOA after supplementation with collagen peptides. However, the significance of the results is limited due to possible biases such as small sample sizes and inconsistencies within the included studies. The confidence in the effect estimates for the outcome pain using GRADE is rated as moderate and for ‚adverse effects‘ as very low (29).
Another clinical application of collagen is via local injections, which has already shown positive outcomes in various musculoskeletal conditions, e.g. in patients with KOA (14-19) and tendonitis (30).
Tarantino et al. (2023) categorize intra-articular administration of type I collagen as effective in reducing symptoms and improving function in patients with KOA based on the results of seven studies. In some cases, no side effects occurred, while in other studies, moderate reactions to the injections and pain at the injection sites were reported. Long-term follow-up and further in vitro and in vivo research are advocated to confirm the results so that the effects of type I collagen as an intra-articular treatment for KOA can be understood in detail (31). Due to the risk of bias in the individual studies, the results should be critically scrutinized and consistently placed in the context of the entire literature.
Exemplary Comparison of Collagen Products
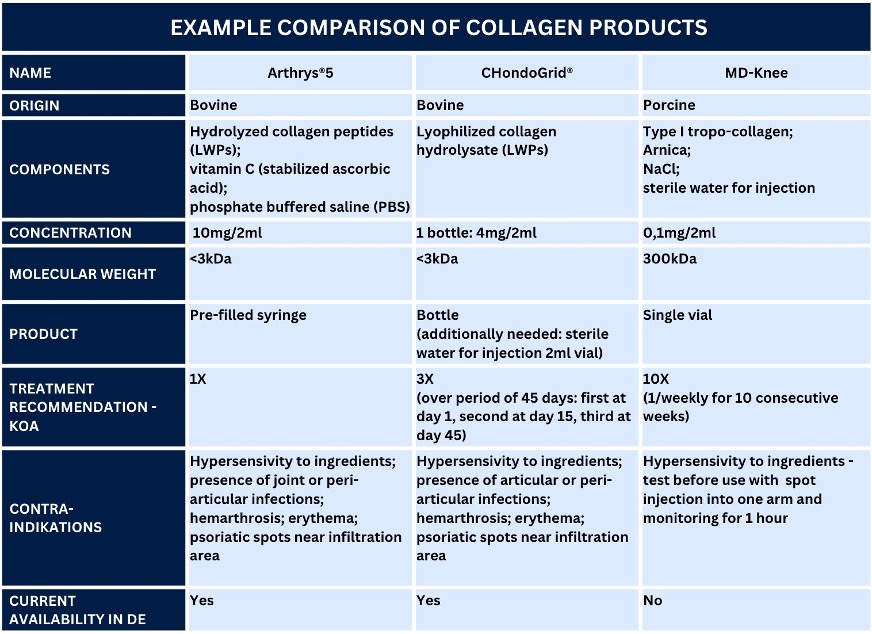
Table 1 shows an exemplary comparison of collagen products for the musculoskeletal system using the example of intra-articular injections. Some manufacturers also offer other products in adapted formulations for other indications. This comparison focuses on the products Arthrys®, CHondroGrid® and MD-Knee due to the availability of information. However, a recent review also listed other products such as Cartifill, CartiZol and Fibroquel (23).
The table shows differences between the available products for intra-articular injections, e.g. in terms of origin (bovine/porcine) and molecular weights (<3kDa/300kDa). While Arthrys®5 and MD-Knee are ready-to-use injectables, CHondroGrid® must be mixed with sterile water for injections before administration. Before the respective application, the individual manufacturer’s instructions for the products must be checked and followed strictly.
A comprehensive preparation for the application of Orthobiologics and hygienically correct work under aseptic conditions are mandatory to minimize the risk of complications and infection (see Herstellerangaben, Hygieneleitlinien zu Punktion und Injektion der KRINKO und S-1 Leitlinie Intraartikuläre Punktionen und Injektionen: Hygienemaßnahmen – in Überarbeitung, AWMF) (2,32,33).
Case Report: Knee – Cartilage Damage
First experiences from the practical application of intra-articular collagen injections in sports medicine have been documented. A 60-year-old male patient (former professional athlete) with symptomatic KOA and cartilage damage (femoropatellar III°-IV°) re-introduced himself in our clinic. The patient initially presented with severe knee pain (VAS 6-7/10) after prolonged walking (>3 km) and was severely restricted in his daily activities. After comprehensive initial diagnostics, the patient began intensive medical training therapy to improve the muscular stabilization of the knee joint (personal training by sports scientists – supervised training recommended AAOS – Guideline 2021). Adjuvant therapy with intra-articular injections to improve mobility and joint function, relieve pain and promote regeneration completed the treatment concept.
- Day 0: (diagnostics: joint inflammation -> aspiration of synovial fluid); 1 intra-articular HA injection (high molecular weight) under sonographic guidance
- Day 7: 1 intra-articular HA injection (high molecular weight) under sonographic guidance
- Day 14: (diagnostics: no joint inflammation or joint effusion); 1 intra-articular PRP injection (low leukocyte) under sonographic guidance
Following the first treatment cycle, the patient’s quality of life improved due to significantly reduced pain when walking longer distances.
The patient reported local pain behind the patella at the next appointment following a hiking vacation. Therefore, alternative treatment options were presented.
- Day 28: (diagnostics: no joint inflammation or joint effusion); 1 intra-articular injection of collagen sonographic guidance
The patient received an intra-articular injection of Arthrys® 5mg/2ml. Three days later, the patient reported a significant reduction in pain when walking (VAS 2/10) and was able to resume his normal daily activities. This condition was maintained for three months.
Conclusion
The combination therapy of Orthobiologics may improve conservative treatment options and shows promising effects in enhancing patient outcomes. Treatment algorithms are currently developed to identify possible treatment synergisms and enable the most effective synergisms based on the assumed mode of action and the presumed effects of different available products in combination with the first clinical experiences.
The challenge moving forward to advance Orthobiologics in sports medicine will be identifying and evaluating optimal formulations and combinations of available treatments for the most appropriate clinical indications.
High-quality research is urgently needed to support the current presumptions and treatment ideas. Therefore, it remains essential for clinicians to critically evaluate the treatment options individually and to stay informed about the latest research findings and evidence-based recommendations.
Literature
- Makaram NS, Safran MR, Abrams GD, Sherman SL, Murray IR. Rationale for the Use of Orthobiologics in Sports Medicine. Oper Tech Sports Med. 1. September 2020;28(3):150753.
- Moreno-Garcia A, Rodriguez-Merchan EC. Orthobiologics: Current role in Orthopedic Surgery and Traumatology. Arch Bone Jt Surg. Juli 2022;10(7):536–42.
- Angele P, Buchhorn T, Zellner J. Orthobiologics in der klinischen Anwendung. Thema Neuer Kniechirurgie Innov Knee Surg. 1. Dezember 2022;38(4):424–30.
- Obana KK, Schallmo MS, Hong IS, Ahmad CS, Moorman CT 3rd, Trofa DP, u. a. Current Trends in Orthobiologics: An 11-Year Review of the Orthopaedic Literature. Am J Sports Med. September 2022;50(11):3121–9.
- Mavrogenis AF, Karampikas V, Zikopoulos A, Sioutis S, Mastrokalos D, Koulalis D, u. a. Orthobiologics: a review. Int Orthop. Juli 2023;47(7):1645–62.
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. Dezember 2020;29–30:100587.
- Xie F, Kovic B, Jin X, He X, Wang M, Silvestre C. Economic and Humanistic Burden of Osteoarthritis: A Systematic Review of Large Sample Studies. PharmacoEconomics. November 2016;34(11):1087–100.
- Hussain ZB, Chahla J, LaPrade RF, Mandelbaum BR. Orthobiologics: Today and Tomorrow. In: Farr J, Gomoll AH, Herausgeber. Cartilage Restoration: Practical Clinical Applications [Internet]. Cham: Springer International Publishing; 2018. S. 131–42. Verfügbar unter: https://doi.org/10.1007/978-3-319-77152-6_11
- DGOU. Gonarthrose (Living Guideline) S2k-Leitlinie – Deutsche Gesellschaft für Orthopädie und Unfallchirurgie e.V. 29. Februar 2024; Verfügbar unter: https://register.awmf.org/de/leitlinien/detail/033-004
- Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A. Intra-articular Corticosteroid Injections in the Hip and Knee: Perhaps Not as Safe as We Thought? Dezember 2019;293(3).
- Hirsch G, Kitas G, Klocke R. Intra-articular corticosteroid injection in osteoarthritis of the knee and hip: factors predicting pain relief–a systematic review. Semin Arthritis Rheum. April 2013;42(5):451–73.
- McAlindon TE, LaValley MP, Harvey WF, Price LL, Driban JB, Zhang M, u. a. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA. 16. Mai 2017;317(19):1967–75.
- Kamel SI, Rosas HG, Gorbachova T. Local and Systemic Side Effects of Corticosteroid Injections for Musculoskeletal Indications. AJR Am J Roentgenol. März 2024;222(3):e2330458.
- De Luca P, Colombini A, Carimati G, Beggio M, de Girolamo L, Volpi P. Intra-Articular Injection of Hydrolyzed Collagen to Treat Symptoms of Knee Osteoarthritis. A Functional In Vitro Investigation and a Pilot RetrospectiveClinical Study. J Clin Med. 4. Juli 2019;8(7).
- Volpi P, Zini R, Erschbaumer F, Beggio M, Busilacchi A, Carimati G. Effectiveness of a novel hydrolyzed collagen formulation in treating patients with symptomatic knee osteoarthritis: a multicentric retrospective clinicalstudy. Int Orthop. Februar 2021;45(2):375–80.
- Furuzawa-Carballeda J, Lima G, Llorente L, Nuñez-Álvarez C, Ruiz-Ordaz BH, Echevarría-Zuno S, u. a. Polymerized-type I collagen downregulates inflammation and improves clinical outcomes in patients with symptomatic knee osteoarthritis following arthroscopiclavage: a randomized, double-blind, and placebo-controlled clinical trial. ScientificWorldJournal. 2012;2012:342854.
- Martin Martin LS, Massafra U, Bizzi E, Migliore A. A double blind randomized active-controlled clinical trial on the intra-articular use of Md-Knee versus sodium hyaluronate in patients with knee osteoarthritis(„Joint“). BMC Musculoskelet Disord. 22. Februar 2016;17:94.
- Reshkova V, Rashkov R, Nestorova R. EFFICACY AND SAFETY EVALUATION OF GUNA COLLAGEN MDs INJECTIONS IN KNEE OSTEOARTHRITIS − A CASE SERIES OF 30 PATIENTS. Physiological Regulating Medicine. 2016;27–9.
- Lee HS, Oh KJ, Moon YW, In Y, Lee HJ, Kwon SY. Intra-articular Injection of Type I Atelocollagen to Alleviate Knee Pain: A Double-Blind, Randomized Controlled Trial. Cartilage. Dezember 2021;13(1_suppl):342S-350S.
- Luu Thi B, Tran Thi L, Hang Hoang Thi M. Effectiveness of Hydrolyzed Collagen Peptide Injection for the Treatment of Collateral Ligament Pain: A Randomized Controlled Trial. Journal of Clinical & Medical Surgery. 2023;3(2).
- Gallo N, Natali ML, Sannino A, Salvatore L. An Overview of the Use of Equine Collagen as Emerging Material for Biomedical Applications. J Funct Biomater. 1. November 2020;11(4).
- Salvatore L, Gallo N, Natali ML, Terzi A, Sannino A, Madaghiele M. Mimicking the Hierarchical Organization of Natural Collagen: Toward the Development of Ideal Scaffolding Material for Tissue Regeneration. Front Bioeng Biotechnol. 2021;9:644595.
- Salvatore L, Natali ML, Brunetti C, Sannino A, Gallo N. An Update on the Clinical Efficacy and Safety of Collagen Injectables for Aesthetic and Regenerative Medicine Applications. Polymers. 17. Februar 2023;15(4).
- Wang H. A Review of the Effects of Collagen Treatment in Clinical Studies. Polymers. 9. November 2021;13(22).
- Sorushanova A, Delgado LM, Wu ZN, Shologu N, Kshirsagar A, Raghunath R, u. a. The Collagen Suprafamily: From Biosynthesis to Advanced Biomaterial Development. Advanced Materials. 2019;(31):1–39.
- Martínez-Puig D, Costa-Larrión E, Rubio-Rodríguez N, Gálvez-Martín P. Collagen Supplementation for Joint Health: The Link between Composition and Scientific Knowledge. Nutrients [Internet]. 2023;15(6). Verfügbar unter: https://www.mdpi.com/2072-6643/15/6/1332
- Elango J, Hou C, Bao B, Wang S, Maté Sánchez de Val JE, Wenhui W. The Molecular Interaction of Collagen with Cell Receptors for Biological Function. Polymers. 23. Februar 2022;14(5).
- Campos LD, Santos Junior V de A, Pimentel JD, Carregã GLF, Cazarin CBB. Collagen supplementation in skin and orthopedic diseases: A review of the literature. Heliyon. April 2023;9(4):e14961.
- Lin CR, Tsai SHL, Huang KY, Tsai PA, Chou H, Chang SH. Analgesic efficacy of collagen peptide in knee osteoarthritis: a meta-analysis of randomized controlled trials. J Orthop Surg. 16. September 2023;18(1):694.
- Uroz NZ. COLLAGEN MEDICAL DEVICE INFILTRATIONS IN SHOULDER PATHOLOGIES. CALCIFIC SUPRASPINATUS TENDINITIS. Physiological Regulating Medicine. 2016;15–7.
- Tarantino D, Mottola R, Palermi S, Sirico F, Corrado B, Gnasso R. Intra-Articular Collagen Injections for Osteoarthritis: A Narrative Review. Int J Environ Res Public Health. 1. März 2023;20(5).
- Labmayr V, Eckhart FJ, Smolle M, Klim S, Fischerauer SF, Bernhardt G, u. a. Sterile Punktion großer Gelenke. Oper Orthop Traumatol. 1. Februar 2023;35(1):65–80.
- Infektionsprävention (KRINKO). Kommentar zur Empfehlung „Anforderungen an die Hygiene bei Punktionen und Injektionen“. Robert Koch-Institut; 2021. S. 13–15.
- TISS’YOU S.r.l. Arthrys – Regenerative peptides [Internet]. TISS’YOU S.r.l; Verfügbar unter: https://www.tissyou.com/wp-content/uploads/2020/11/Arthrys_brochure_web_pagine-singole-ENG.pdf
- Bioteck S.p.A. CHondroGrid – The new collagen way. Innovative und progressive Behandlungsmethode bei Chondropathie. Produktinformation SpongioTech; o.A..
- Guna S.p.a. Manual of Injection Therapy for the Musculoskeletal System. 2022.
Autoren
ist Facharzt für Orthopädie und Unfallchirurgie, Spezielle Unfallchirurgie und Sportmedizin. Er ist Gründer und Inhaber des LANS Medicum. Seine mannschaftsärztlichen Betreuungen umfassten u. a. das Handballteam des HSV sowie von 2011-2014 die Erstligafußballmannschaft des Hamburger SV. Heute betreut er mit seinem Team mehrere Fußball- und Hockeyteams sowie das Hamburger Ballett von John Neumeier. Außerdem ist Prof. Catalá-Lehnen als Professor für den Schwerpunkt Orthopädie an der Medical School Hamburg und am UKE in der Lehre für das Fach Knochenpathologie tätig.
ist Sportphysiotherapeutin und GCP-zertifizierte (AMG und MPDG) Studienkoordinatorin. Sie ist Head of Science am LANS Medicum Hamburg, studierte in Hamburg und Plymouth (UK) und schloss mit einem MSc Advanced Professional Practice in Physiotherapy mit dem Schwerpunkt Clinical Research ab.
Studium der Humanmedizin an der LMU München, Bern und VR China. Facharzt für Neurologie, spezielle Schmerztherapie und Rehabilitationswesen, Dozent und Ausbilder für Ärzte in der Schmerztherapie. Medizinischer Direktor für diverse Firmen.
© Andreas Kuhrau





