Diagnostic thermography has now achieved a relevant status for assessing functional symptoms in sports orthopaedics. Trigger points are readily shown with the help of thermal imaging cameras, especially chronified functional symptoms in the entire axial skeleton, and corresponding therapeutic measures such as shock wave treatments, dry needling, cryotherapy, friction massage or taping can be started and their success monitored in the course of treatment.
With the infrared thermography we use (FLIR E75 thermal imaging camera, Fig. 1) the camera displays more than 75,000 measured positions with a thermal sensitivity of <0.04 degrees temperature difference, and thus it can reliably demonstrate even small areas of hyperaemia (trigger points). We can differentiate between active myofascial trigger points which are often extremely painful and frequently weaken the affected muscle, latent myofascial trigger points which are only painful on movement, and associated trigger points which develop due to functional disorders of neighbouring muscle groups. More recently, differentiated EMG investigations are being used increasingly in conjunction with thermography to identify problems with efferent signals to the musculature in parallel, and to correct these with the help of biofeedback training. Initially thermography was mainly used for muscles close to the vertebral column to identify painful muscular tension in the lumbar and cervical spine and to work specifically on these structures. In the present case the indication for diagnostic thermography has been extended to Achilles tendon symptoms.
Case study
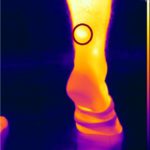
We were consulted by a 29-year-old [female] patient with recurrent symptoms at the myotendinous junction of the right Achilles tendon, particularly one day after sporting activity (running). Her average training schedule was 40 – 50 km/week, she could not remember having had an accident. The diagnostic imaging we performed (ultrasound, MRI) and differentiated foot pressure measurements ruled out any structural changes in the tendon and any relevant foot deformities. Only the ultrasonography on the day after sporting activity showed peritendinitis in the proximal part of the tendon. The subsequent EMG of the gastrocnemius muscle showed an increased resting tone of the right gastrocnemius. Further functional diagnostics (neuromuscular activation) showed a reduced efferent supply to the medial calf muscles (Figs. 2 & 3).
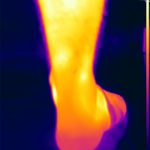
The thermography carried out in parallel impressively showed a painful area in the proximal region of the right Achilles tendon (Figs. 4 & 5). In addition to (focused) shockwave therapy the patient was treated with laser therapy and neuroreflex cryotherapy of the proximal Achilles tendon origin with taping of the muscle and (later) adjunctive biofeedback training of the calf muscles (Figs. 6 – 10).
The follow-up examinations showed a marked reduction in trigger point formation over the proximal Achilles tendon, even after the first treatment session. After two sessions of shockwave therapy plus taping and two sessions of biofeedback training the patient was clinically 100% symptom-free (Figs. 11 – 13).
Summary
Thermography impressively helps diagnose muscular trigger points and monitor successful treatment, particularly of functional symptoms, including those in the tendinous origins distant from the spine. Secondary muscle dysfunction is demonstrated by EMG and treated using EMG-based biofeedback therapy.
Autoren
ist Leiter von Ortho4Sport in Köln. Er ist Facharzt für Chirurgie mit Zusatzbezeichnungen Sportmedizin und Chirotherapie. Außerdem ist Professor Tobolski Verbandsarzt des Tennisverbandes Mittelrhein sowie ATP-Turnierarzt.