As already described in a previous article in the sportärztezeitung, COVID 19 can cause endothelial changes and induce systemic disease [1]. If an athlete becomes infected with SARS-CoV2, this is especially significant in terms of myocardial involvement. Equally relevant is the observation that transient myocardial changes can develop even after recovery from a Covid-19 infection.
Hanneman, Hubois and Schoffel published a cohort study in January 2022 in which PET imaging suggested evidence of myocarditis subsequent to a COVID-19 infection [2]. It was in this context that Gänsslen et al. developed a return to play protocol for the German ice hockey league [1] that sought to return athletes to their sport as safely as possible, depending on the symptoms and medical findings. The following presents and interprets the study findings in a team who largely became infected with SARS-CoV2.
Baseline
25 of a team of 32 active male professional athletes (80 %) aged 18 – 60 became infected with SARS-CoV-2 within the 11 days following a shared bus journey of several hours. The cohort comprised solely those actively engaged in sports, i.e. only players and trainers were included in the cohort. Others in immediate contact with the squad (staff) were excluded, even though further positive and negative cases of Covid were identified in those in the team’s environment. After the initial positive rapid antigen test, diagnosis was confirmed with a PCR test. The CT values in the tests were between 14.88 and 29.7. In some tests, there was molecular genetic evidence of an N501Y mutation without an L452R mutation, indicating an Omicron variant, specifically SARS-CoV-2 B1.1.529. At the time of the infection, everybody in the cohort was considered as vaccinated or recovered. Two of the infected athletes were considered as having received a booster shot.
The vaccination/recovery status in detail was as follows:
- 20 had received two doses of the Pfizer/Biontech vaccine
- 1 had received two doses of the Astra Zeneca vaccine
- 4 had received one dose of the Johnson and Johnson vaccine
- 1 had received two doses of the Johnson and Johnson vaccine
- 2 had received two doses of the Moderna vaccine
- 1 had received one dose each of the Moderna and Pfizer/Biontech vaccine
- 1 was considered as recovered and had received one dose of the Pfizer/Biontech vaccine
- 2 had been considered as recovered since October
- 3 were considered as having received one Pfizer/Biontech booster vaccine in the period
up to seven days prior to infection
Study findings
As the return to play protocol provides for a medical examination post recovery and the scope of the tests is based on the symptoms and physical examination, but in this case well over half the team were infected, it was decided to conduct an initial examination in the course of the infection. This first involved performing a medical history and physical examination. A blood sample was then taken. The following blood parameters were determined:
- basic blood count and additional differential blood count
- iron
- CK, CK-MB
- GOT, GPT, γ-GT, ALP, GLDH, total bilirubin
- creatinine, GFR
- NT-proBNP, Troponin T
- ferritin
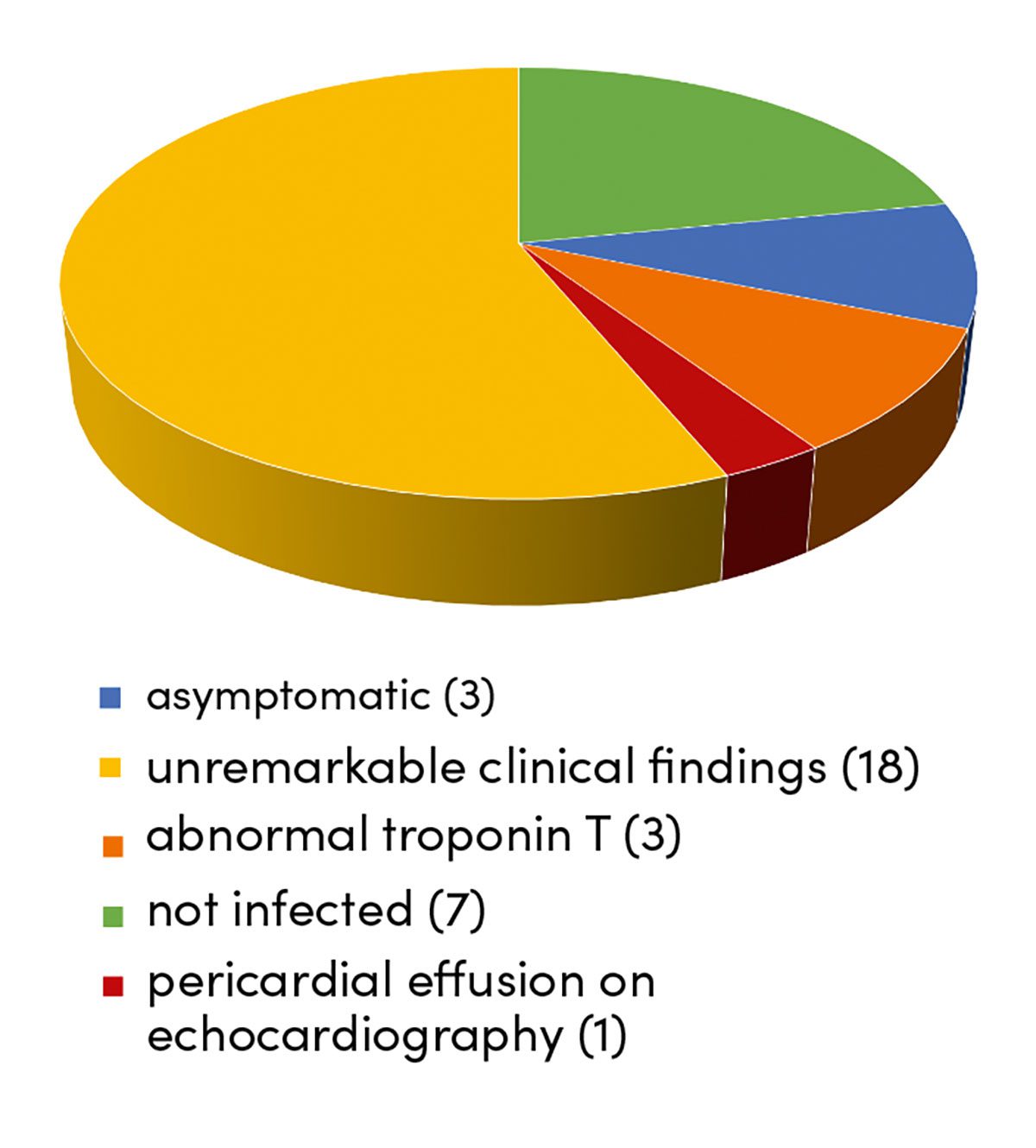
These tests and examinations were performed between 3 and 8 days post infection. When their medical history was taken 3 of the cohort stated that they were asymptomatic. The remaining 22 athletes reported symptoms ranging from mild irritation of the pharynx and larynx to fever, night sweats, dyspnoea, hyperhidrosis and dizziness. At no point did any of the patients require hospitalisation. The auscultation findings for the heart and lungs in the physical examination were unremarkable. In laboratory tests, however, there was a noticeable CRP increase above 5 mg/L in 3 of the cohort, an elevated troponin T level above 0.014 ng/mL in a further 3 patients and a CK-MB of 33 with a total CK of 219 U/L, equivalent to 15 %, in one other patient. Although a further 4 patients also had an elevated CK-MB level, total CK was normal. This finding was accordingly considered as not clinically relevant, though it is a matter of debate as to whether this might nevertheless indicate irritation of the myocardium. A monocyte count of between 10 and 21 % was found in 15 athletes, in 2 of whom neutropenia was also identified (40 %, 37 % and 28 %). The findings for transaminase and kidney parameters in clinical chemistry did not provide any useful indications.
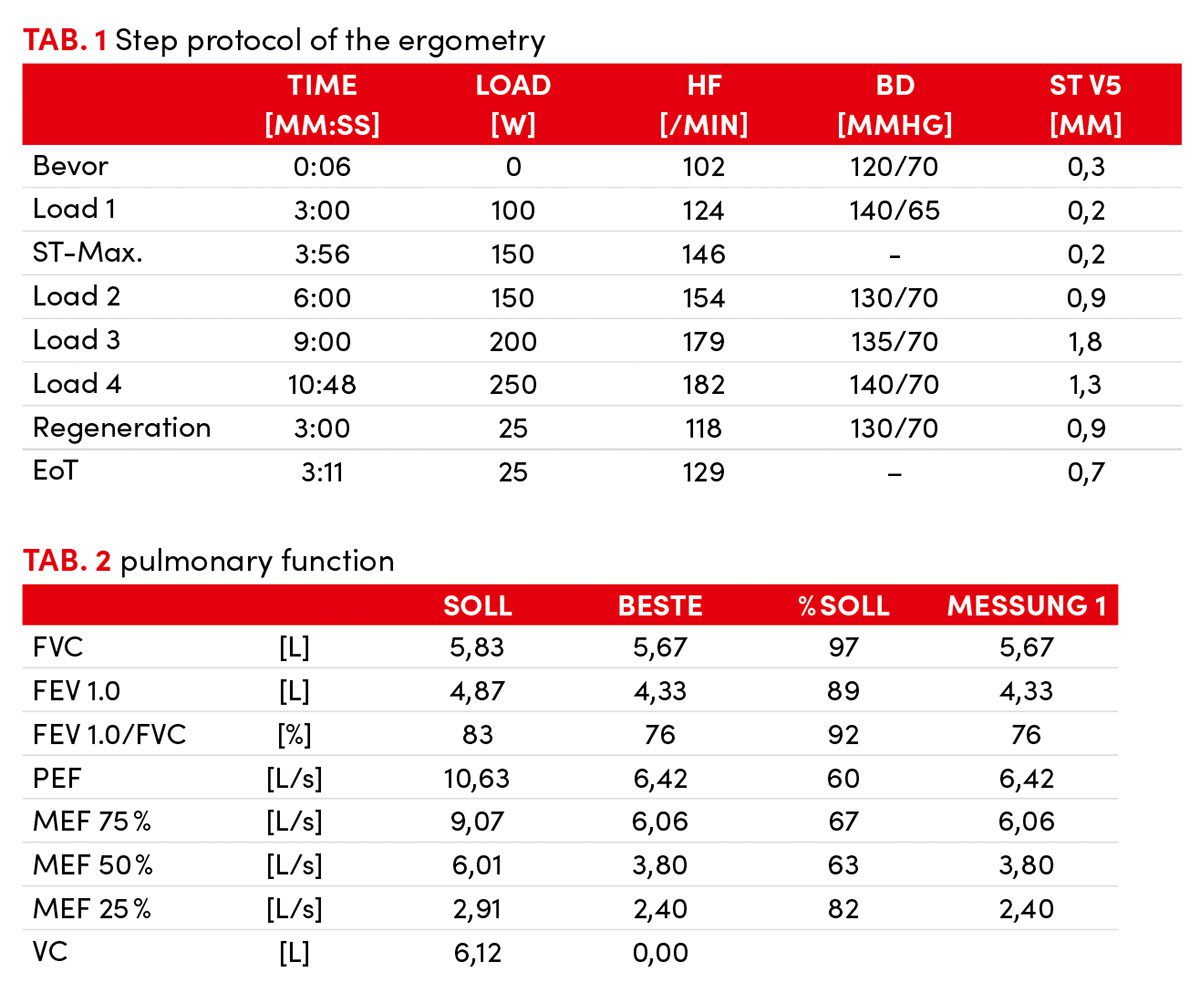
The symptoms of all patients improved in the following 10 days. Follow-up tests and examinations were provided to the infected patients subsequent to the quarantine imposed by the authorities. The procedure followed was based on the return to play protocol. Fortunately, no clinically relevant arrhythmias were identified in the resting ECG and ergometry (up to a max. of 450 W) (Tab. 1 – ergometer step protocol).
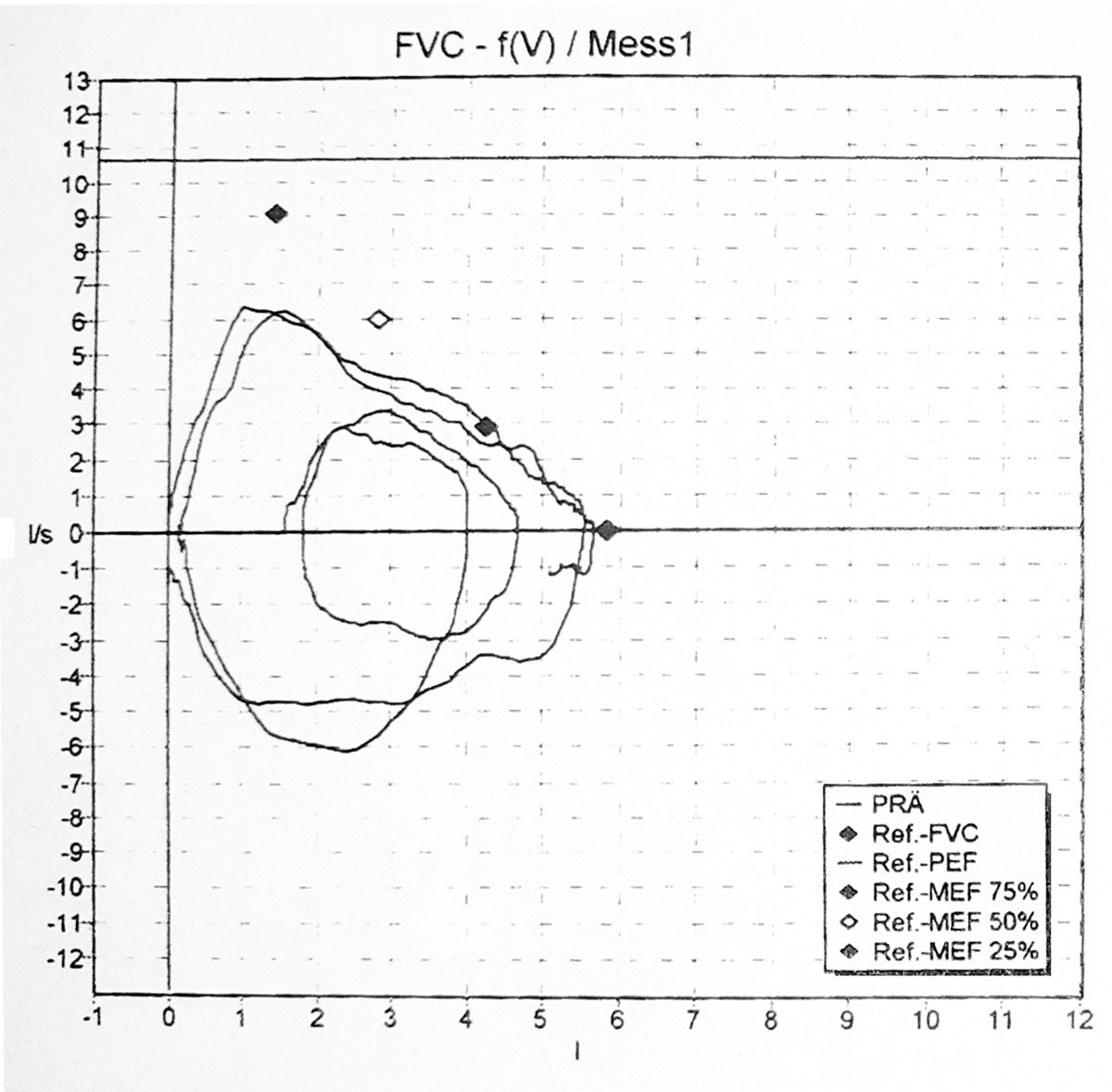
The results of laboratory tests also indicated regression. Although the findings of the pulmonary function tests conducted were normal, they nevertheless indicated loss of function when compared to the pulmonary status in the preseason physical fitness test (Fig. 1 (pulmonary function test), Table 2 (pulmonary function)). In the case of the athletes this means that in the preseason physical fitness test the lung volumes of each athlete were markedly greater than those of a normal patient. The follow-up test after quarantine now showed reduced function when compared to the preseason test but one which was nevertheless classified as “normal”.
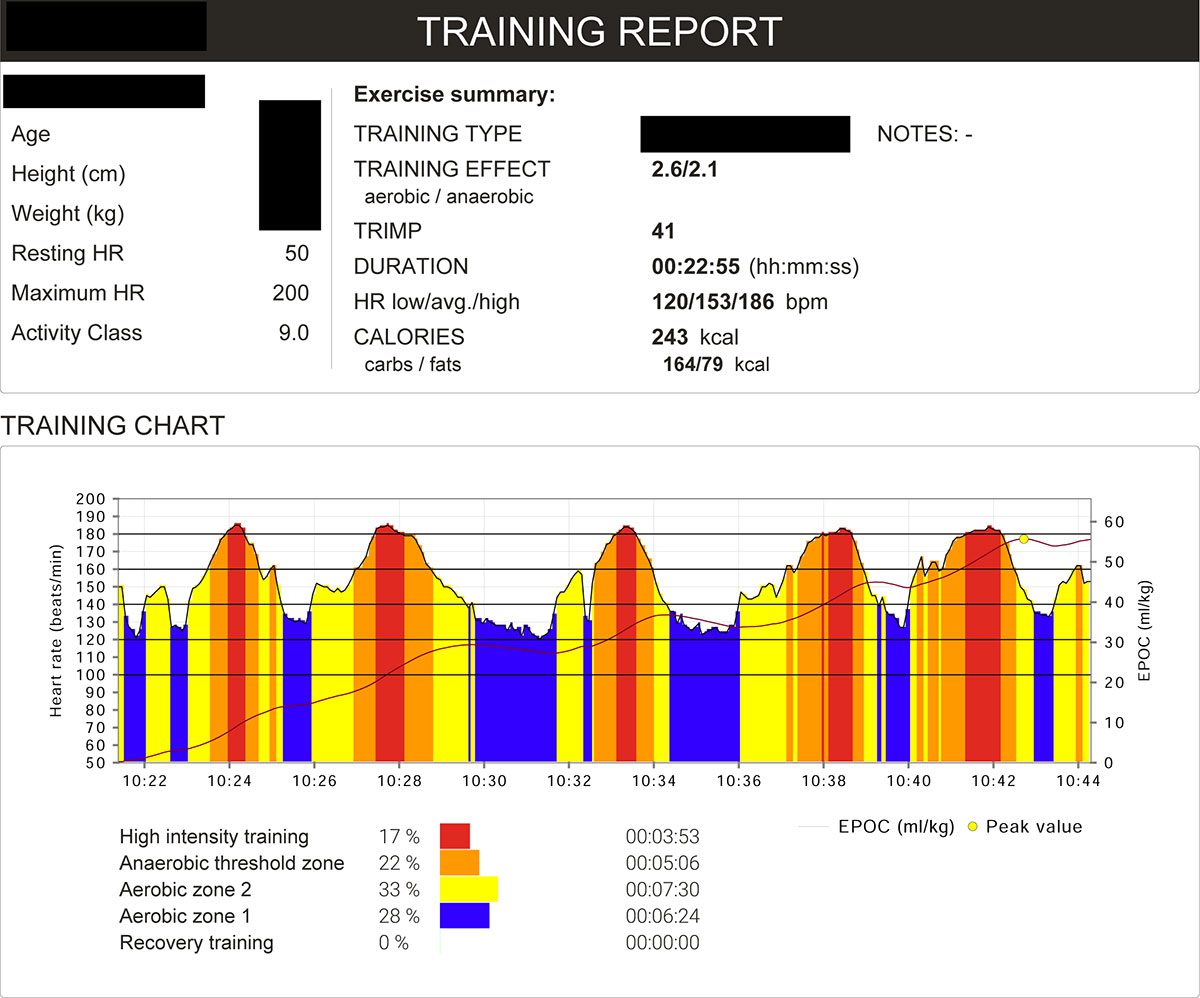
An echocardiography was performed in 15 patients. This was indicated in patients with either positive troponin T, elevated CK-MB, previous fever or elevated resting pulse rate. A mild, haemodynamically nonsignificant pericardial effusion was detected in one patient 18 days after a positive PCR test. This finding also regressed in the further course. Three athletes with elevated troponin T or a persistent markedly elevated resting pulse rate underwent cardiac MRI. Fortunately, none of the findings indicated any pathology. A chest X-ray in PA and laterally was performed post Covid infection in one patient with persistent cough and dyspnoea. The cardiopulmonary findings were unremarkable with no indication of pneumonia. As the symptoms regressed in the further course, it was not considered necessary to perform a chest CT scan to detect milk glass opacities. On completion of the tests and examinations, all the athletes were able to begin the reintegration part of the return to play protocol. This lasted on average 7-10 days. As loading was gradually increased, one athlete complained of dyspnoea and another of dizziness at high loads. The return to play protocol was adjusted accordingly. The heart rates determined by the HR belt worn at each training session were similarly too high for the respective load provided for in the protocol. The training intensity had to be adjusted for 2 – 4 days (Figs. 2, 3).
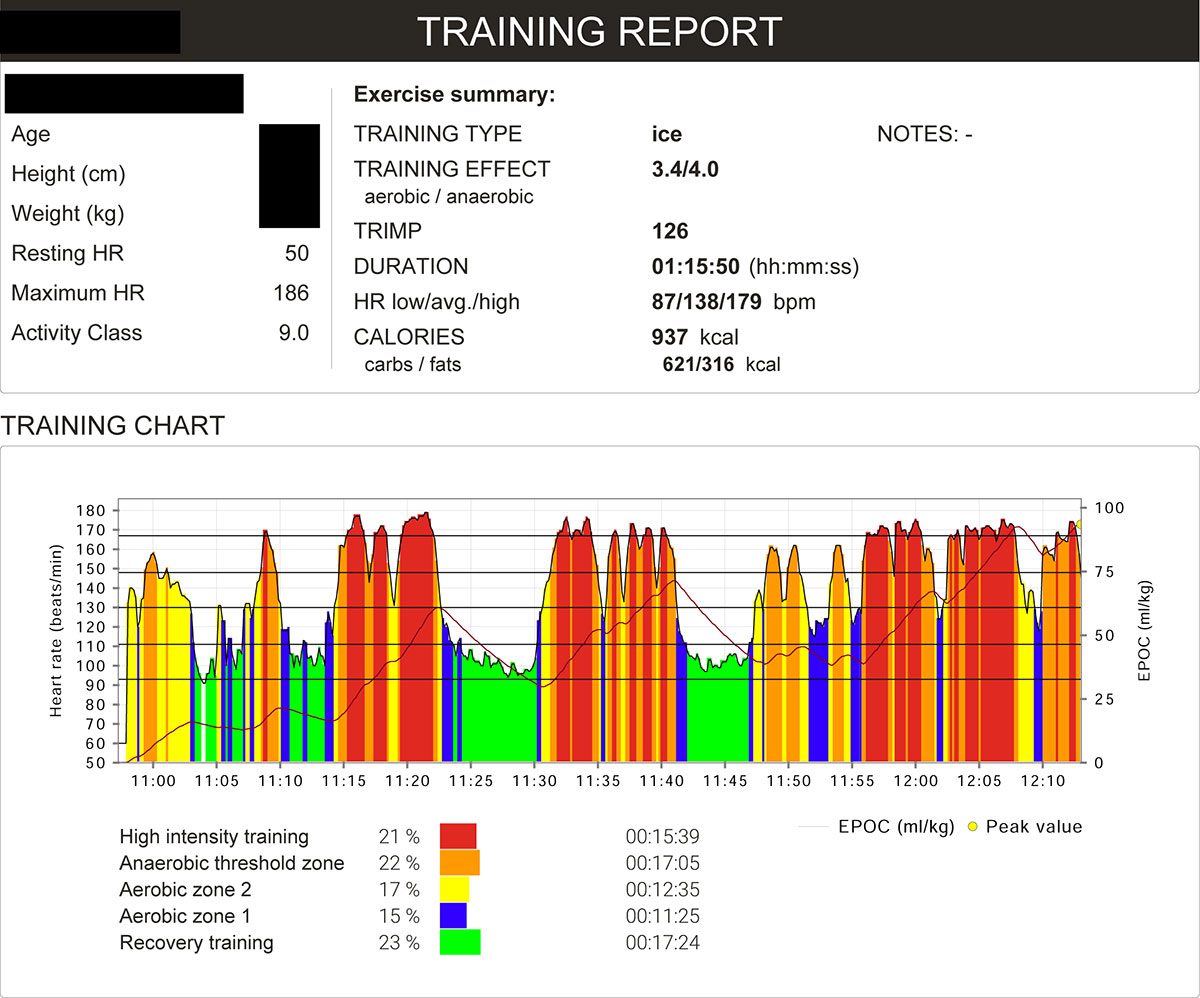
Fig. 2 training report 1
Summary and discussion
25 of a team of 32 men (80 %) actively engaged in sport and aged 18 – 60 became infected with SARS-Covid-CoV2 although all of them had either previously recovered from the infection or had been vaccinated or had received a booster shot against it. Of those who became infected, only 3 (12 %) were asymptomatic and 3 (12 %) were found to have an elevated troponin T level. Mild pericardial effusion was initially identified in one person (4 %). Of the 3 athletes who had received a booster shot, one did not become infected and the other two reported only mild symptoms (Fig. 4). Due to the small size of the cohort it was not considered necessary to establish individual vaccination status in relation to the severity of the course of the disease.
All the infected athletes became infected even though they had either recovered from the infection or been vaccinated against it. Although vaccination does seem to provide protection against a severe course, this is not sufficient to prevent infection with the Omicron variant. As cardiac involvement cannot be ruled out in a SARS-CoV-2 infection, even if the patient is asymptomatic and has been fully vaccinated, and is likely to be detected in laboratory tests and imaging, it is recommended that patients actively engaged in sports be closely monitored subsequent to a Covid-19 infection to minimise the risks of cardiac affection to the fullest possible extent. Laboratory diagnostics including troponin T and a resting ECG at minimum are recommended in addition to the physical examination. If a patient had developed a fever during the course of the infection, it seems sensible to perform further laboratory diagnostics. In patients with an elevated troponin T level or echocardiography abnormalities, in my judgement, particularly considering previous test and examination findings for recovered patients, even in those who were reportedly asymptomatic, the indication for cardiac MRI should be liberally interpreted.
As a study on 789 athletes by Martinez et al. published in March 2021 confirms, implementation of a return to play protocol noticeably reduced the risk associated with training loads in sports subsequent to a Covid-19 infection [3]. As in this case athletes became infected with the Omicron variant despite being vaccinated and there was suspicion of cardiac involvement, the return to play protocol available to the German ice hockey league (Penny-DEL) as a guideline should be regularly discussed and adjusted. The cohort data collected shows that the Omicron variant of the Covid 19 virus can also impact different organ systems in those who have recovered or been vaccinated, the risks of which can be noticeably reduced by systematic monitoring and individual adjustment of the scope of examinations and training tests as part of reintegration into sports.
Literatur
[1] Gänsslen, A., et al., Return to Play nach COVID-19. sportärztezeitung, 01/2021. https://sportaerztezeitung.com/rubriken/kardiologie/6575/return-to-play-nach-covid-19/
[2] Hannemann, K., et al., Combined Cardiac Fluorodeoxyglucose–Positron Emission Tomography/Magnetic Resonance Imaging Assessment of Myocardial Injury in Patients Who Recently Recovered From COVID-19. JAMA Cardiol., 2022. doi:10.1001/jamacardio.2021.5505
[3] Martinez, M. Et al.,Prevalence of Inflammatory Heart Disease Among Professional Athletes With Prior COVID-19 Infection Who Received Systematic Return-to-Play Cardiac Screening. JAMA Cardiol. 2021;6(7):745 – 752. doi:10.1001/jamacardio.2021.0565
Expert Talk
Our scientific advisor, Felix Post MD, Medical Director of Internal Medicine/Cardiology at the Catholic Hospital of Coblenz-Montabaur, where he is also the head of the Corona task force, had the opportunity to read the article by Jochen Veit MD before publication and discussed it with him, as one expert to another.
Unser wissenschaftlicher Beirat PD Dr. med. Felix Post, Chefarzt der Inneren Medizin/Kardiologie am Katholischen Klinikum Koblenz-Montabaur, wo er zusätzlich die Corona-Taskforce leitet, hat sich den Artikel von Dr. med. Jochen Veit schon vorab angeschaut und sich mit ihm darüber von Experte zu Experte unterhalten. Article…
Autoren
ist Facharzt für Allgemeinmedizin mit Zusatzbezeichnungen Sportmedizin, Chirotherapie
und Präventivmedizin mit eigener Praxis (gemeinsam mit Frank Emschermann) in Nordwalde. Außerdem ist er Teamarzt der Iserlohn Roosters (Eishockey DEL).