Authors:
ROBERT BIELITZKI, TOM BEHRENDT, PROF. LUTZ SCHEGA / DEPARTMENT OF SPORT SCIENCE, OTTO-VON-GUERICKE UNIVERSITY MAGDEBURG
PROF. MICHAEL BEHRINGER MD / DEPARTMENT OF SPORTS SCIENCES, GOETHE UNIVERSITY FRANKFURT
ALEXANDER FRANZ MD / DEPARTMENT OF ORTHOPEDICS AND TRAUMA SURGERY, UNIVERSITY HOSPITAL BONN
Acute severe injuries and degenerative diseases of the musculoskeletal system as well as surgical interventions are usually characterized by phases of restricted mobility with strongly reduced load-bearing capacity or complete immobility of corresponding areas [1]. This temporary or long-lasting situations are strongly associated with strength loss due to neural impairments (e.g., decline in high threshold motor unit recruitment and arthrogenic inhibition [2, 3]) and muscle atrophy (due to an imbalance in muscle protein synthesis and breakdown [3, 4]).
In the recent past, a new conservative therapy approach termed blood flow restriction (BFR) has gained great interest from scientists and therapists. BFR training describes an alternative method based on partial vascular occlusion to induce metabolic changes that allow mitigating functional and morphological degeneration or increasing muscle mass and strength by using no additional activities [5] or low mechanical loads [6], respectively. Considering these beneficial effects, BFR seems suitable after acute injuries (e.g., anterior cruciate ligament rupture) as well as for patients with degenerative diseases (e.g., gonarthrosis) or after a surgical intervention (e.g., total knee arthroplasty).
Mechanisms of BFR-induced effects on muscular adaptations and pain management
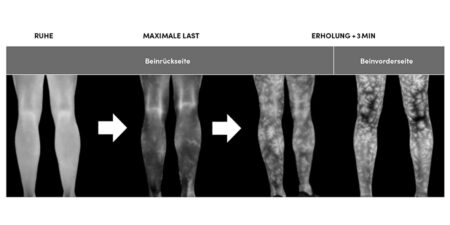
BFR is characterized by the application of pneumatic cuffs to the proximal part of a limb to decrease arterial and block venous blood flow [7]. Venous blood pooling is thought to increase metabolic stress due to a change in energy metabolism in favor of anaerobic processes and accumulating metabolites [8, 9], which accelerates muscle fatigue development [10]. In this regard, invasive catheter studies demonstrated that low-load resistance exercise under venous occlusion causes hypoxemia in the exercising limb [11]. Further occurring mechanisms (e.g., increased type II muscle fiber recruitment and cell swelling) are assumed to trigger signal cascades which increase protein synthesis and thus, induce muscle hypertrophy [8, 9]. In addition, BFR is able to reduce pain due to provoking hypoalgetic effects [12]. Considering the current evidence, BFR-induced hypoalgesia is probably caused by a conditioned pain modulation [13] (i.e., diffuse noxious inhibitory control-like effect [14] or “pain inhibits pain” [15]) where a reduction in pain perception is evoked by another heterotopically applied noxious stimulus [16]. Another possible mechanism is the activation of the endogenous opioid and endocannabinoid systems due to stimulation of group III and IV afferents leading to the production of specific neurotransmitters, which modulate the sensitivity of nociceptors [17, 18].
BFR in clinical practice in phases of immobilization or severely restricted mobility
Preoperative treatment of degenerative diseases and/or elective surgery
Considering the main benefits of BFR training, inducing significant adaptations in the muscular system with the associated ability to reduce pain, its application in the medical field is of particular interest. Joint arthrosis is one of the major diseases affecting the skeletal system, leading to severe reductions in mobility as well as in skeletal muscle mass and strength [19, 20]. Total joint replacement (e.g., total knee arthroplasty, TKA) is often the last option to maintain or restore mobility. However, the surgery itself and early postoperative immobilization usually causes further progression of muscular atrophy and strength loss [21]. Therefore, an improvement in patients’ functional and morphological resources before elective surgeries such as TKA is a strong predictor for a better postoperative outcome [22, 23]. While previous attempts about prehabilitation (i.e., exercise programs prior to a surgery) showed too small and/ or only short-term effects in improving postoperative function and reducing pain after joint replacement surgery [24], BFR could provide a decisive new alternative to create a favorable functional and morphological environment before surgery. Prehabilitative treatment with BFR training has already been shown to have a major impact on pre- and postoperative muscle mass, strength and function in patients receiving elective TKA [25] or abdominal surgery [26].
Postoperative treatment or conservative rehabilitation
In the early postoperative period, especially during complete immobilization, BFR can be used passively (i.e., without additional exercise) to counteract the injury/ surgery-induced loss of muscle mass [27], strength [28, 29], and to reduce local pain [30]. If possible, resistance exercises with very low loads can be performed during phases of limited mobility. It has been shown that low-load BFR training induces similar increases in muscle mass to high-load [6] and low-load training performed until exhaustion [31]. In this regard, especially low-load BFR training might be a convenient option as high mechanical stress of high-load training is avoided and cumulative low mechanical stress of low-load training until exhaustion is reduced (i.e., due to lower total work) [32]. Furthermore, Korakakis et al. have shown that BFR combined with low load knee extension exercise not only reduced anterior knee pain but also allowed the patients tolerate higher mechanical loads in subsequent therapy sessions [14, 33] which, in turn, favors gains in muscle strength. Therefore, Bielitzki et al. proposed that an early integration of BFR potentially accelerates the recovery process compared to traditional care [32].
Safety information
Generally, there is no increased risk of adverse health events when performing BFR training [34]. Apart from side effects of traditional exercise/ training (e.g., muscle damage/ soreness), the most common adverse events are tingling sensations in distal extremities (71.2 %), hematomas (4.8 – 13.1 %), and numbness (1.3 – 26.9 %). In few cases, serious side effects such as rhabdomyolysis (0.01 – 1.9 %) or venous thrombus formation (0.06 %) may occur [35, 36]. However, BFR exercise may cause an increased response of the metabolic and cardiovascular systems (lactic acidosis, venous hypertension) [37, 38]. To minimize the risk of adverse health events, patients should be screened for possible contraindications (Table 1). However, if used appropriately, BFR can also be applied in critically ill patients (e.g., patients with chronic kidney [39] or cardiovascular disease [40]).

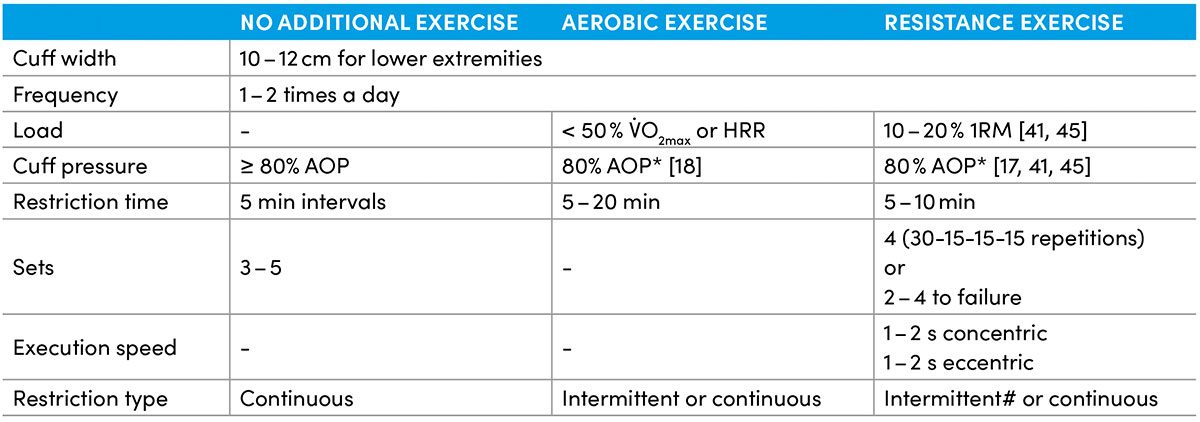
Recommendations for application during strongly reduced load capacity
Considering the current recommendations, Table 2 provides guidance for the proper application of BFR training during immobilization and strongly limited mobility with very low-load tolerance with the goal of optimizing training efficacy and patient safety [34]. Especially in these phases, it seems necessary to set an adequate high level of cuff pressure in order to induce beneficial effects. For example, Mouser et al. have shown that only high pressures combined with very low-load resistance training induced beneficial vascular adaptations similar to high-load resistance training [41]. Furthermore, the studies by Hughes et al. demonstrated that high pressures are more likely to induce hypoalgetic effects than low pressures combined with low-load resistance and aerobic exercise [17, 18].
Conclusion
Considering the current evidence on muscle mass and strength in clinical populations [42, 43], BFR provides a promising method for patients especially during immobility or periods of strongly reduced mobility with very low mechanical resilience. While a preoperative treatment can create a protective effect on the surgical limb to reduce post-surgical strength loss and muscle atrophy [3], post-injured / post-surgical therapy can be supported by the application of BFR, either passive or combined with very low-load exercises, to regain pre-traumatic / presurgical strength level faster compared without using BFR [32].
Literature
- You DZ, Leighton JL, Schneider PS. Current Concepts in Rehabilitation Protocols to Optimize Patient Function Following Musculoskeletal Trauma. Injury. 2020;51 Suppl 2:S5-S9. doi:10.1016/j.injury.2020.03.047.
- Campbell M, Varley-Campbell J, Fulford J, Taylor B, Mileva KN, Bowtell JL. Effect of Immobilisation on Neuromuscular Function In Vivo in Humans: A Systematic Review. Sports Med. 2019;49:931–50. doi:10.1007/s40279-019-01088-8.
- Patterson SD, Hughes L, Owens J. Early Postoperative Role of Blood Flow Restriction Therapy to Avoid Muscle Atrophy. In: Noyes FR, Barber-Westin S, editors. RETURN TO SPORT AFTER ACL RECONSTRUCTION AND OTHER KNEE OPERATIONS: Limiting. [S.l.]: SPRINGER NATURE; 2019. p. 261–274. doi:10.1007/978-3-030-22361-8_12.
- Atherton PJ, Greenhaff PL, Phillips SM, Bodine SC, Adams CM, Lang CH. Control of skeletal muscle atrophy in response to disuse: clinical/preclinical contentions and fallacies of evidence. Am J Physiol Endocrinol Metab. 2016;311:E594-604. doi:10.1152/ajpendo.00257.2016.
- Cerqueira MS, Do Nascimento JDS, Maciel DG, Barboza JAM, Brito Vieira WH de. Effects of blood flow restriction without additional exercise on strength reductions and muscular atrophy following immobilization: A systematic review. J Sport Health Sci. 2020;9:152–9. doi:10.1016/j.jshs.2019.07.001.
- Lixandrão ME, Ugrinowitsch C, Berton R, Vechin FC, Conceição MS, Damas F, et al. Magnitude of Muscle Strength and Mass Adaptations Between High-Load Resistance Training Versus Low-Load Resistance Training Associated with Blood-Flow Restriction: A Systematic Review and Meta-Analysis. Sports Med. 2018;48:361–78. doi:10.1007/s40279-017-0795-y.
- Mattocks KT, Jessee MB, Mouser JG, Dankel SJ, Buckner SL, Bell ZW, et al. The Application of Blood Flow Restriction: Lessons From the Laboratory. Curr Sports Med Rep. 2018;17:129–34. doi:10.1249/JSR.0000000000000473.
- Pearson SJ, Hussain SR. A review on the mechanisms of blood-flow restriction resistance training-induced muscle hypertrophy. Sports Med. 2015;45:187–200. doi:10.1007/s40279-014-0264-9.
- Jessee MB, Mattocks KT, Buckner SL, Dankel SJ, Mouser JG, Abe T, Loenneke JP. Mechanisms of Blood Flow Restriction: The New Testament. Techniques in Orthopaedics. 2018;33:72–9. doi:10.1097/BTO.0000000000000252.
- Husmann F, Mittlmeier T, Bruhn S, Zschorlich V, Behrens M. Impact of Blood Flow Restriction Exercise on Muscle Fatigue Development and Recovery. Med Sci Sports Exerc. 2018;50:436–46. doi:10.1249/MSS.0000000000001475.
- Franz A, Berndt F, Raabe J, Harmsen J-F, Zilkens C, Behringer M. Invasive Assessment of Hemodynamic, Metabolic and Ionic Consequences During Blood Flow Restriction Training. Front Physiol. 2020;11:617668. doi:10.3389/fphys.2020.617668.
- Bielitzki R, Behrendt T, Behrens M, Schega L. Blutflussrestriktionstraining zur akuten und chronischen Schmerzreduktion in der orthopädischen Rehabilitation. B&G Bewegungstherapie und Gesundheitssport. 2022;38:96–102. doi:10.1055/a-1815-8426.
- Hughes L, Patterson SD. Low intensity blood flow restriction exercise: Rationale for a hypoalgesia effect. Med Hypotheses. 2019;132:109370. doi:10.1016/j.mehy.2019.109370.
- Korakakis V, Whiteley R, Epameinontidis K. Blood Flow Restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Phys Ther Sport. 2018;32:235–43. doi:10.1016/j.ptsp.2018.05.021.
- Yarnitsky D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol. 2010;23:611–5. doi:10.1097/ACO.0b013e32833c348b.
- Sirucek L, Ganley RP, Zeilhofer HU, Schweinhardt P. Diffuse noxious inhibitory controls and conditioned pain modulation: a shared neurobiology within the descending pain inhibitory system? Pain 2022. doi:10.1097/j.pain.0000000000002719.
- Hughes L, Patterson SD. The effect of blood flow restriction exercise on exercise-induced hypoalgesia and endogenous opioid and endocannabinoid mechanisms of pain modulation. J Appl Physiol. 2020;128:914–24. doi:10.1152/japplphysiol.00768.2019.
- Hughes L, Grant I, Patterson SD. Aerobic exercise with blood flow restriction causes local and systemic hypoalgesia and increases circulating opioid and endocannabinoid levels. J Appl Physiol. 2021;131:1460–8. doi:10.1152/japplphysiol.00543.2021.
- Barber-Westin S, Noyes FR. Blood Flow-Restricted Training for Lower Extremity Muscle Weakness due to Knee Pathology: A Systematic Review. Sports Health. 2019;11:69–83. doi:10.1177/1941738118811337.
- Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol. 2000;27:1745–52.
- Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003;21:775–9. doi:10.1016/S0736-0266(03)00052-4.
- Mizner RL, Petterson SC, Stevens JE, Axe MJ, Snyder-Mackler L. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. J Rheumatol. 2005;32:1533–9.
- Zeni JA, Snyder-Mackler L. Preoperative predictors of persistent impairments during stair ascent and descent after total knee arthroplasty. J Bone Joint Surg Am. 2010;92:1130–6. doi:10.2106/JBJS.I.00299.
- Wang L, Lee M, Zhang Z, Moodie J, Cheng D, Martin J. Does preoperative rehabilitation for patients planning to undergo joint replacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2016;6:e009857. doi:10.1136/bmjopen-2015-009857.
- Franz A, Ji S, Bittersohl B, Zilkens C, Behringer M. Impact of a Six-Week Prehabilitation With Blood-Flow Restriction Training on Pre- and Postoperative Skeletal Muscle Mass and Strength in Patients Receiving Primary Total Knee Arthroplasty. Front Physiol. 2022;13:881484. doi:10.3389/fphys.2022.881484.
- Wooten SV, Fleming RYD, Wolf JS, Stray-Gundersen S, Bartholomew JB, Mendoza D, et al. Prehabilitation program composed of blood flow restriction training and sports nutrition improves physical functions in abdominal cancer patients awaiting surgery. Eur J Surg Oncol. 2021;47:2952–8. doi:10.1016/j.ejso.2021.05.038.
- Takarada Y, Takazawa H, Ishii N. Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med Sci Sports Exerc. 2000;32:2035–9. doi:10.1097/00005768-200012000-00011.
- Kubota A, Sakuraba K, Sawaki K, Sumide T, Tamura Y. Prevention of disuse muscular weakness by restriction of blood flow. Med Sci Sports Exerc. 2008;40:529–34. doi:10.1249/MSS.0b013e31815ddac6.
- Kubota A, Sakuraba K, Koh S, Ogura Y, Tamura Y. Blood flow restriction by low compressive force prevents disuse muscular weakness. J Sci Med Sport. 2011;14:95–9. doi:10.1016/j.jsams.2010.08.007.
- Pereira FEC, Mello IL, Pimenta FHdOM, Costa DM, Wong DVT, Fernandes CR, et al. A Clinical Experimental Model to Evaluate Analgesic Effect of Remote Ischemic Preconditioning in Acute Postoperative Pain. Pain Research and Treatment. 2016;2016:5093870. doi:10.1155/2016/5093870.
- Farup J, Paoli F de, Bjerg K, Riis S, Ringgard S, Vissing K. Blood flow restricted and traditional resistance training performed to fatigue produce equal muscle hypertrophy. Scand J Med Sci Sports. 2015;25:754–63. doi:10.1111/sms.12396.
- Bielitzki R, Behrendt T, Behrens M, Schega L. Time to Save Time: Beneficial Effects of Blood Flow Restriction Training and the Need to Quantify the Time Potentially Saved by its Application during Musculoskeletal Rehabilitation. Phys Ther 2021. doi:10.1093/ptj/pzab172.
- Korakakis V, Whiteley R, Giakas G. Low load resistance training with blood flow restriction decreases anterior knee pain more than resistance training alone. A pilot randomised controlled trial. Phys Ther Sport. 2018;34:121–8. doi:10.1016/j.ptsp.2018.09.007.
- Patterson SD, Hughes L, Warmington S, Burr J, Scott BR, Owens J, et al. Blood Flow Restriction Exercise: Considerations of Methodology, Application, and Safety. Front Physiol. 2019;10:533. doi:10.3389/fphys.2019.00533.
- Queiros VS de, Dantas M, Neto GR, Da Silva LF, Assis MG, Almeida-Neto PF, et al. Application and side effects of blood flow restriction technique: A cross-sectional questionnaire survey of professionals. Medicine (Baltimore). 2021;100:e25794. doi:10.1097/MD.0000000000025794.
- Nakajima T, Kurano M, Iida H, Takano H, Oonuma H, Morita T, et al. Use and safety of KAATSU training:Results of a national survey. Int. J. KAATSU Ttaining Res. 2006;2:5–13. doi:10.3806/ijktr.2.5.
- Spranger MD, Krishnan AC, Levy PD, O’Leary DS, Smith SA. Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol. 2015;309:H1440-52. doi:10.1152/ajpheart.00208.2015.
- da Cunha Nascimento D, Schoenfeld BJ, Prestes J. Potential Implications of Blood Flow Restriction Exercise on Vascular Health: A Brief Review. Sports Med. 2020;50:73–81. doi:10.1007/s40279-019-01196-5.
- Corrêa HL, Neves RVP, Deus LA, Souza MK, Haro AS, Costa F, et al. Blood Flow Restriction Training Blunts Chronic Kidney Disease Progression in Humans. Med Sci Sports Exerc. 2021;53:249–57. doi:10.1249/MSS.0000000000002465.
- Cahalin LP, Formiga MF, Owens J, Anderson B, Hughes L. Beneficial Role of Blood Flow Restriction Exercise in Heart Disease and Heart Failure Using the Muscle Hypothesis of Chronic Heart Failure and a Growing Literature. Front Physiol. 2022;13:924557. doi:10.3389/fphys.2022.924557.
- Mouser JG, Mattocks KT, Buckner SL, Dankel SJ, Jessee MB, Bell ZW, et al. High-pressure blood flow restriction with very low load resistance training results in peripheral vascular adaptations similar to heavy resistance training. Physiol Meas. 2019;40:35003. doi:10.1088/1361-6579/ab0d2a.
- Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD. Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med. 2017;51:1003–11. doi:10.1136/bjsports-2016-097071.
- Perera E, Zhu XM, Horner NS, Bedi A, Ayeni OR, Khan M. Effects of Blood Flow Restriction Therapy for Muscular Strength, Hypertrophy, and Endurance in Healthy and Special Populations: A Systematic Review and Meta-Analysis. Clin J Sport Med. 2022;32:531–45. doi:10.1097/JSM.0000000000000991.
- Brandner CR, May AK, Clarkson MJ, Warmington SA. Reported Side-effects and Safety Considerations for the Use of Blood Flow Restriction During Exercise in Practice and Research. Techniques in Orthopaedics. 2018;33:114–21. doi:10.1097/BTO.0000000000000259.
- Dankel SJ, Jessee MB, Buckner SL, Mouser JG, Mattocks KT, Loenneke JP. Are higher blood flow restriction pressures more beneficial when lower loads are used? Physiol Int. 2017;104:247–57. doi:10.1556/2060.104.2017.3.2.
Autoren
Department of Orthopedics and Trauma Surgery, University Hospital Bonn.