Infrared Thermography (IRT) allows quantifying the skin temperature by measuring the energy radiated by the human body [20]. IRT is based on a camera that creates colourful images, where every pixel contains a temperature data (fig. 1). This method is used visually and objectively (extracting metrics) to support diagnosis, prevent and follow-up injuries.

Basic concepts
Temperature and health are two concepts that have been closely related to each other for centuries [18]. From the time of Hippocrates, health professionals have recognised the importance of a raised temperature. Fever is, with no doubt, an universal symptom of unhealthy status that is currently a trending topic because of the Covid-19 pandemic [24]. From a physiological point of view, the human body manages its challenging thermoregulation by the central nervous system from the hypothalamus [13]. We find different ways to transfer the excess of heat from the human body: evaporation, conduction, convection and radiation. About 60 % of human heat loss is accounted for by radiation, and this is exactly what we measure when we use IRT. Therefore, IRT provides us with information on the physiological and metabolic state of the structures and tissues closest to the skin.
Influence factors and thermal asymmetries
The main limitation of the application of IRT in humans is the large number of factors that affect the skin temperature. We classify them into three main groups: environmental, technical and individual factors [4]. According to the principle of homeostasis, the human body has a thermal balance between the bilateral regions [12]. For this curious reason, and given that most of the influence factors are bilaterally affected, the search for thermal asymmetries is the best option to determine the normality of a thermal image [3]. In this sense, it has been determined that a thermal asymmetry between contralateral regions of interest (ROI) greater than 0.3º C should be considered as abnormal [9]. To sum up, if we want to avoid the majority of influence factors that affect the interpretation of human thermography, we should focus on thermal asymmetries rather than absolute temperatures. In other words, it is not that important if the right knee is 28º C or 32º C, but if it is 1º C warmer than the left.
Methodology and protocol
IRT gives us the possibility of using two methodologies: the qualitative (visual analysing) and the quantitative (objective metrics) ones. Both methods are perfectly valid and complementary. The qualitative method allows us to quickly and intuitively analyse colours to detect abnormalities in the thermogram at a glance. However, this is a subjective method and the colours can be modified. The interpretation depends on colour contrast that might be under or overestimated. On the other hand, the quantitative method lets us to objectively quantify the metrics obtained in each pixel (for instance, a 320 x 240 thermogram has 76.800 pixels). This second method requires image processing, which can be realized manually. The fastest and most reliable results can be reached using software solutions that process thermal images automatically [17]. Additionally, it is recommended to follow the guidelines set by Gomes-Moreira and collaborators [7] with the TISEM protocol, which offer a checklist to reassure the quality on the thermal data collection.
Main sports medicine applications
Of all current IRT applications, we highlight three main uses: injury prevention, diagnosis support and injury follow-up [3].
1. Injury prevention
There is more and more evidence confirming that IRT is a useful strategy to reduce and prevent injuries [14, 23]. The most interesting results have been performed with soccer teams [2, 9]. Both studies compared a first period with a second one using a thermography protocol. In the case of the Brazilian team, Côrte and collaborators showed a 64 % reduction in muscle injuries [2]. In case of a LaLiga Spanish team the percentage was similar and significant: 70 % less muscle injuries in the second period [9]. In both works, IRT was a key tool for prevention. It was essential that the whole staff was coordinated to implement an intervention protocol based on the thermal asymmetries, either to reduce the workload or establish an individualized treatment [9].
2. Diagnosis support
As mentioned before, the reputation of IRT has been clearly damaged by its use as a unique tool for the diagnosis of pathologies, especially breast cancer [15]. Although it is true that the efficacy of IRT has been demonstrated for the diagnosis of some rheumatic, diabetic and even liver pathologies [13], in most cases it is advisable to complement the thermal examination with another type of imaging or diagnostic tests. However, it is true that IRT stands out for being much faster and cheaper than other imaging technologies such as magnetic resonance or x-rays [22]. IRT allows determining the nature of an injury or pathology before evaluating it with more expensive, slow and invasive tests. In this sense, one of the most fascinating things about IRT and the thermal behaviour of an injury was described in the study of Sillero and collaborators [21]. Those authors described the thermal profile of more than 200 cases according to location, damaged tissue and pathology. The main conclusion was that most of the lesions occur with hyperthermia (+ 0,5º C warmer), but injuries related to the nervous, vascular and muscular system generated precisely the opposite: hypothermia. This nuance is key to determining which test is necessary to confirm a diagnosis and, therefore, concludes that IRT saves time and money, as well as the invasiveness of certain tests to the patient [21].
3. Injury follow-up
Probably the most effective IRT application is the injury follow-up. IRT allows us to visualize and quantify the thermal asymmetries generated by an injury during the recovery period, so that we can closely follow the evolution of the affected area until it returns to normal values. IRT is also valid to control the possible compensations that an injury produces in the rest of the body, information that is a key factor for the rehabilitation and reduction of chances of injury relapse [5]. We can find different studies analysing the utility of IRT by monitoring different injuries: ACL rupture [16], ankle sprain [11] or bone fracture [25]. The work of Fernández-Cuevas and del Estal describes how thermal asymmetries evolve throughout the rehabilitation period in the most common injuries in football players [5]. The findings described in these works are especially interesting both from a clinical point of view and for rehabilitation and return to play approach in the sports field [5].
Thermography diagnosis support case study: Plantar fasciitis vs nervous issue
Plantar heel pain is a very common symptom among high performance and amateur athletes. We normally relate this pain to plantar fasciitis, which is, in most of the cases, a correct diagnosis. In this case study, we will show how IRT helped to reconsider a plantar fasciitis case based on the thermal results.
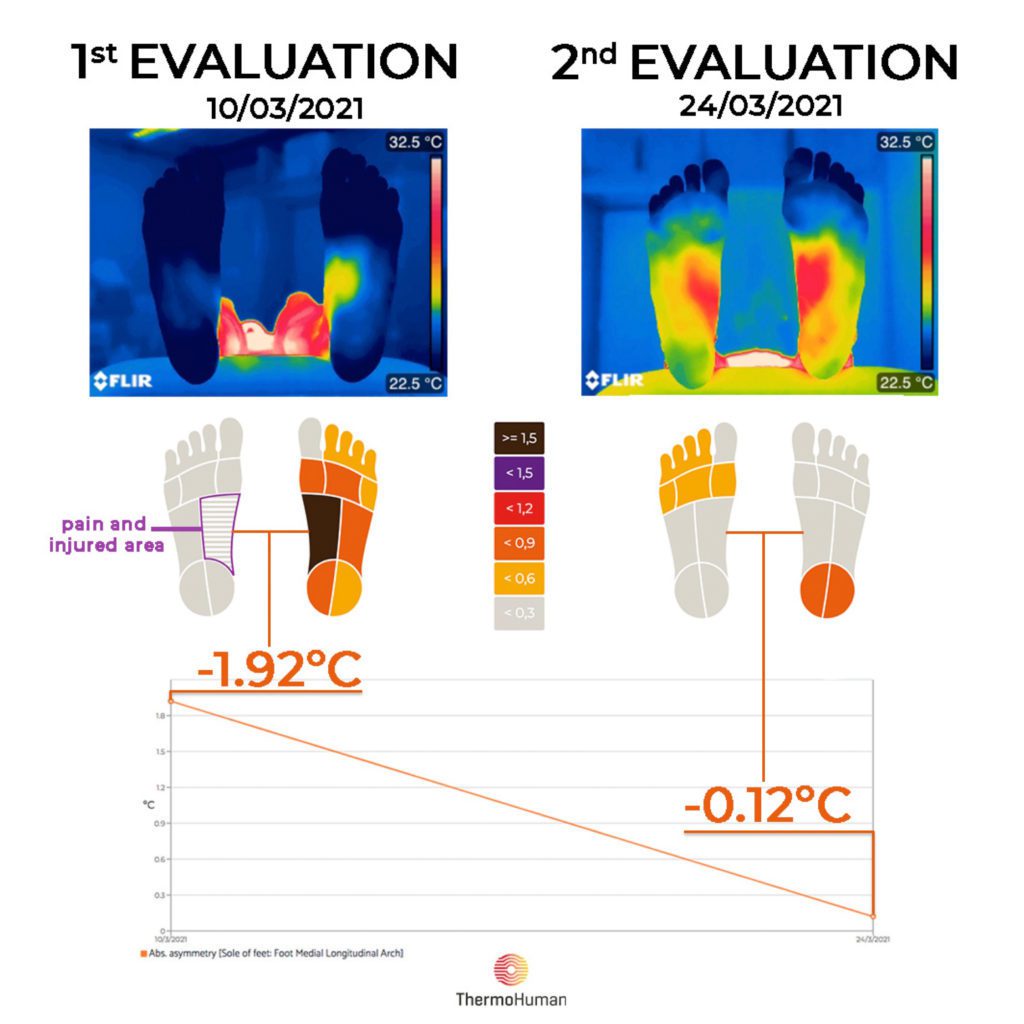
This is the case study of a female athlete (25 years old), specialized in 800 m, that was diagnosed at the end of 2020 with plantar fasciitis in her right foot. The symptoms were compatible with the diagnosis (plantar heel pain, more intense in the early morning or after resting, etc.). Extended physiotherapy treatment, shockwave therapy and Laserneedle therapy were applied over 12 weeks. In addition to that, she also got insoles. Unfortunately, all these interventions did not improve the situation and she was not able to return to train because her plantar heel pain did not disappear. The first thermography evaluation was performed following TISEM consensus [7] on the 10th March 2021, more than 2 months after the diagnosis. At that stage, the athlete did not refer pain -she could do some strength and swimming training-, but heel contact or running were painful activities (5/10 in a NRS pain scale): she was not able to run in the previous 8 weeks. When taking the foot sole thermal image, we asked her to point at the painful region (fig. 2).

As we mentioned previously, depending on the injury/pathology and the involved tissue, the thermal response might be different [21]. In this case, plantar fasciitis is pathology linked to a hyperthermic response [8]. Thus, we expected to find a warmer right heel but we found a colder one (fig. 3, representing the thermal image and asymmetries analyzed by ThermoHuman with –1.92º C colder right inner arch). These thermal results forced us to recommend the reconsideration of the diagnosis. Bearing in mind the shown hypothermic pattern (characteristic from nervous issues), we suggested to explore potential differential diagnosis related to nerve syndromes (such as the Baxter’s neuropathy or Inferior Calcaneal Nerve compression).
A study performed in the UK reported that 12,1 % of all musculoskeletal foot and ankle consultations in primary care in 2006 were related to heel pain, with 7,5 % of them specifying plantar fasciitis [26]. That means that not all plantar heel pain can be diagnosed as a plantar fasciitis. Indeed, Buchbinder showed some differential diagnosis of plantar heel pain, among them we find several nerve issues [1].
In light of the new information, the diagnosis was reviewed and a right ankle block was found. After mobilization of the blockage, there was an immediate release of pain. As a result, she started running again pain free (she only reported a mild tingling sensation, which may in fact be an indicator that the nerve was affected). Two weeks after the first evaluation, we repeated the assessment with the athlete (24th March 2021). By this second thermal evaluation, we observed that the injured and painful area (the right foot medial longitudinal arch) presented a no significant –0.12º C asymmetry, which means a thermal asymmetry decrease of 1.80º C from the first to the second evaluation (14 days). This evolution can be seen on figure 3.
CONCLUSIONS
Despite the factors that influence IRT, it has been shown that when used with an appropriate protocol, methodology and tools, IRT can be useful for injury prevention, diagnosis support and injury follow-up. These benefits can be accentuated when IRT is combined with other technologies, allowing the optimization of diagnostic and recovery processes, and consequently saving time and money.
We showed in this case study how IRT is a valid tool to support heel pain diagnosis. Given the frequency of this injury, it can be especially interesting for professionals working in the area of podiatry, physiotherapy and sports medicine. The initial plantar fasciitis diagnosis (hyperthermic pattern) did not agree with the hypothermic pattern found (more linked to nerve issues). After reconsidering the diagnosis and treatment, IRT was additionally helpful to confirm and quantify the significant reduction of the thermal asymmetry (from –1.92º C to –0.12º C). However, we need further research about the thermal behaviour in humans and pathologies/injuries. It represents both a challenge and an obstacle, since for some sceptical professionals IRT has not enough evidence. For others professionals the current results and evidence are not just promising, but already strong enough to benefit from IRT.
TIPP DER REDAKTION ZUM VERTIEFEN
Literatur
- Buchbinder, R. (2004). Plantar Fasciitis. New England Journal of Medicine, 350(21), 2159-2166. doi: 10.1056/NEJMcp032745
- Côrte, A. C., Pedrinelli, A., Marttos, A., Souza, I. F. G., Grava, J., & José Hernandez, A. (2019). Infrared thermography study as a complementary method of screening and prevention of muscle injuries: pilot study. BMJ Open Sport & Exercise Medicine, 5(1), e000431. doi: 10.1136/bmjsem-2018-000431
- Fernández-Cuevas, I., Arnáiz Lastras, J., Escamilla Galindo, V., & Gómez Carmona, P. (2017). Infrared Thermography for the Detection of Injury in Sports Medicine. In J. I. Priego Quesada (Ed.), Application of Infrared Thermography in Sports Science (pp. 81-109). Cham, Switzerland: Springer International Publishing.
- Fernández-Cuevas, I., Bouzas Marins, J. C., Arnáiz Lastras, J., Gómez Carmona, P. M., Piñonosa Cano, S., García-Concepción, M. Á., & Sillero-Quintana, M. (2015). Classification of factors influencing the use of infrared thermography in humans: A review. Infrared Physics & Technology, 71(0), 28-55. doi: http://dx.doi.org/10.1016/j.infrared.2015.02.007
- Fernández-Cuevas, I., & del Estal, A. (2020). Thermal profile description of most common soccer injuries by Infrared Thermography: case studies. Paper presented at the I International Congress on Application of Infrared Thermography in Sport Science, Valencia, Spain.
- Foster, K. R. (1998). Thermographic detection of breast cancer. Ieee Engineering in Medicine and Biology Magazine, 17(6), 10-14. doi: 10.1109/51.734241
- Gomes Moreira, D., Costello, J. T., Brito, C. J., Adamczyk, J. G., Ammer, K., Bach, A. J. E., . . . Sillero-Quintana, M. (2017). Thermographic imaging in sports and exercise medicine: A Delphi study and consensus statement on the measurement of human skin temperature. Journal of Thermal Biology, 69, 155-162. doi: https://doi.org/10.1016/j.jtherbio.2017.07.006
- Gómez Bernal, A., Fernández-Cuevas, I., Alfaro-Santafé, J. J., & Pérez-Morcillo, A. (2020). Termografía infrarroja para la determinación del perfil térmico en fascitis plantar: estudio descriptivo. Revista Española de Podología, 31(Supl1), 1.
- Gómez-Carmona, P. M., Fernández-Cuevas, I., Sillero-Quintana, M., Arnáiz-Lastras, J., & Navandar, A. (2020). Infrared Thermography Protocol on Reducing the Incidence of Soccer Injuries. Journal of Sport Rehabilitation. doi: 10.1123/jsr.2019-0056
- Hillen, B., Pfirrmann, D., Nägele, M., & Simon, P. (2019). Infrared Thermography in Exercise Physiology: The Dawning of Exercise Radiomics. Sports Medicine. doi: 10.1007/s40279-019-01210-w
- Ioannou, S. (2020). Functional Infrared Thermal Imaging: A Contemporary Tool in Soft Tissue Screening. Scientific Reports, 10(1), 9303. doi: 10.1038/s41598-020-66397-9
- Johnson, J. M., & Kellogg, D. L., Jr. (2010). Local thermal control of the human cutaneous circulation. J Appl Physiol, 109(4), 1229-1238. doi: 10.1152/japplphysiol.00407.2010
- Lahiri, B. B., Bagavathiappan, S., Jayakumar, T., & Philip, J. (2012). Medical Applications of Infrared Thermography: A Review. Infrared Physics & Technology, 55(4), 221-235. doi: 10.1016/j.infrared.2012.03.007
- Menezes, P., Rhea, M., Herdy, C., & Simão, R. (2018). Effects of Strength Training Program and Infrared Thermography in Soccer Athletes Injuries. Sports, 6(4), 148.
- Moskowitz, M., Milbrath, J., Gartside, P., Zermeno, A., & Mandel, D. (1976). Lack of Efficacy of Thermography as a Screening Tool for Minimal and Stage I Breast Cancer. New England Journal of Medicine, 295(5), 249-252. doi: 10.1056/NEJM197607292950504
- Piñonosa, S., Sillero-Quintana, M., Milanović, L., Coterón, J., & Sampedro, J. (2013). Thermal evolution of lower limbs during a rehabilitation process after anterior cruciate ligament surgery. Kinesiology, 45(1), 121-129.
- Requena-Bueno, L., Priego-Quesada, J. I., Jimenez-Perez, I., Gil-Calvo, M., & Pérez-Soriano, P. (2020). Validation of ThermoHuman automatic thermographic software for assessing foot temperature before and after running. Journal of Thermal Biology, 92, 102639. doi: https://doi.org/10.1016/j.jtherbio.2020.102639
- Ring, E. F. J. (2007). The historical development of temperature measurement in medicine. Infrared Physics & Technology, 49(3), 297-301.
- Ring, E. F. J. (2010). Beyond human vision: the development and applications of infrared thermal imaging. Imaging Science Journal, The, 58(5), 254-260. doi: 10.1179/174313110X12771950995671
- Ring, E. F., & Ammer, K. (2012). Infrared thermal imaging in medicine. Physiol Meas, 33(3), R33-46. doi: 10.1088/0967-3334/33/3/R33
- Sillero-Quintana, M., Fernández-Jaén, T., Fernández-Cuevas, I., Gómez-Carmona, P. M., Arnaiz-Lastras, J., Pérez, M.-D., & Guillén, P. (2015). Infrared Thermography as a Support Tool for Screening and Early Diagnosis in Emergencies. Journal of Medical Imaging and Health Informatics, 5(6), 1223-1228. doi: 10.1166/jmihi.2015.1511
- Thomas, D., Cullum, D., Siahamis, G., & Langlois, S. (1990). Infrared thermographic imaging, magnetic resonance imaging, CT scan and myelography in low back pain. Br J Rheumatol, 29(4), 268-273.
- Viegas, F., Mello, M., Rodrigues, S., Amaral Costa, C. M., Freitas, L., Rodrigues, E., & Silva, A. (2020). The use of Thermography and its control variables: a systematic review. Revista Brasileira de Medicina do Esporte, 26, 82-86. doi: 10.1590/1517-869220202601217833
- Zhou, Y., Ghassemi, P., Chen, M., McBride, D., Casamento, J., Pfefer, T. J., & Wang, Q. (2020). Clinical evaluation of fever-screening thermography: impact of consensus guidelines and facial measurement location. Journal of Biomedical Optics, 25(9), 097002.
CO-Autoren:
Autoren
International PhD in Sport Sciences (topic: thermography). He is the ThermoHuman cofounder and Sport Scientist. Also he is Injury prevention advisor for football teams as FC Everton, Newcastle United, FC Getafe, FC Villareal or Vfl Wolfsburg among others.



