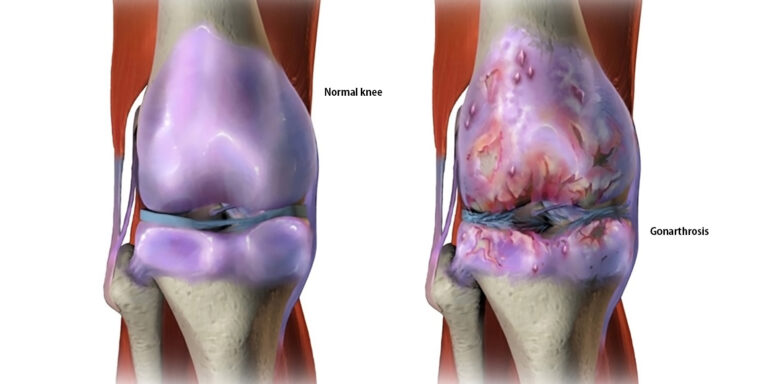
Knee osteoarthritis (gonarthrosis) is one of the most common degenerative joint diseases and a central topic in sports orthopaedic practice. In addition to drug therapies and exercise therapy, dietary supplements are increasingly being used to support joint function. Collagen hydrolysates on the one hand and enzymes with anti-inflammatory effects on the other are particularly in focus.
But how do these substances actually work? Are they absorbed, do they enter the joint systemically – and if so, in what form and by what mechanisms? This article summarizes the current state of research and draws a critical conclusion from the perspective of metabolic biochemistry: What really reaches the knee?
Collagen to support cartilage structure
Basics: Collagen is the most abundant structural protein in the human body (25% of total protein mass). It forms a family of closely related but genetically distinct fiber proteins, with type I being by far the most common. However, type II collagen is mainly found in cartilage. In order to assess the extent to which orally ingested collagen can contribute to the structural development of cartilage, it is important to go into a little more detail here. Collagens consist of three helical peptide chains approximately 1,000 amino acids long, which in turn twist around each other to form a triple helix: the procollagen. The first steps of collagen synthesis take place intracellularly, in the cartilage, where the chondrocyte (the cartilage cell) is responsible for this process. Chondrocytes form groups called chondrons in hyaline cartilage (this type of cartilage forms the joint surfaces). They are embedded in a matrix rich in collagen and chondroitin sulfate, which they synthesize themselves [1]. After secretion of the triple-helix procollagen, both ends are capped extracellularly, forming tropocollagen, which then cross-links to form collagen fibrils – lysine and hydroxylysine at the ends play an important role here. These fibrils assemble into collagen fibers. Each peptide chain, which is 1,000 amino acids long, is synthesized in the chondrocyte on the rough ER: over 300 repetitions of the motif: glycine-X-Y, where X is often proline and Y is often hydroxyproline. However, hydroxyproline is not an independent proteinogenic amino acid but is formed intracellularly by hydroxylation of proline in the peptide chain. The additional OH group allows hydroxyproline to form hydrogen bonds with another strand, enabling the stable triple helix to form. The large number of these hydrogen bonds is responsible for the enormous tensile strength of collagen, which is greater than that of steel. This hydroxylation is dependent on vitamin C. Vitamin C deficiency (e.g., scurvy) therefore leads to a lack of stabilization of newly formed collagen, with symptoms including impaired wound healing, bleeding of the oral mucosa, and others [2].
What happens in the knee?
If we want to do something good for our cartilage and consume collagen, how much of it actually reaches the knee? The collagen subunit tropocollagen already has around 3,000 amino acids, and around 1,000 tropocollagen subunits form a collagen fibril, meaning that a fibril has at least 3 million amino acids. A whole collagen fiber consists of between 10 and 300 fibrils – it quickly becomes clear that neither collagen fibrils, which could attach themselves to other fibrils, nor the tropocollagen subunits, which could cross-link with other tropocolloagens, have any chance of surviving intact (as a helix) in the stomach with the protein-splitting pepsin and the denaturing stomach acid. Even if they did, there are other proteases in the small intestine, and transport from the intestine into the blood can only take place via transporters that carry peptides consisting of a maximum of a few amino acids. Several studies have investigated what actually reaches the knee: it has been proven that small collagen fragments appear in the blood after oral intake and accumulate specifically in cartilage tissue [7, 5]. Oesser et al. (1999) showed in animal studies that radiolabeled gelatin hydrolysates are preferentially stored in joint cartilage [7]. Hydrolyzed collagen is therefore mostly used in dietary supplements – short peptide chains that have been made highly soluble through enzymatic cleavage.

Structural support for cartilage
Preclinical studies suggest that the intake of collagen peptides supports the biomechanical integrity of cartilage and counteracts degenerative processes [8, 9, 12]. So are collagen peptides a direct substrate source for chondrocytes for collagen synthesis? Since protein synthesis at the ribosomes generally only incorporates one amino acid at a time – there is no tRNA for oligopeptides – this is only possible as an indirect effect: The high concentration of precisely those amino acids (from cleaved collagen peptides) that are needed for collagen synthesis ensures increased synthesis performance. There is also no tRNA for hydroxyproline, so that any hydroxyproline from the collagen peptides in the cell is converted back to proline and then hydroxylated to hydroxyproline in the rough ER in a vitamin C-dependent manner. From this perspective, taking hydroxyproline offers no advantages over proline. To summarize: at the structural level, all collagen supplements are simply about increasing the concentration of the amino acids specifically required for collagen. However, it is interesting to note that collagen peptides also appear to have a signaling effect.
Biochemical signaling pathways and anabolic effects
Beyond simply supplying amino acids, certain collagen peptides activate biochemical signaling pathways in chondrocytes. Studies show that the collagen peptide proline-hydroxyproline, for example, can increase the synthesis of hyaluronic acid by synovial cells – a key factor in joint lubrication and viscoelastic protection of cartilage [4]. Further research suggests that collagen peptides have anti-inflammatory effects by inhibiting the NF-κB signaling pathway [6, 8], which can reduce the release of cartilage-degrading enzymes such as MMP-13 [3, 6, 8]. Furthermore, there is evidence that anabolic signaling pathways are involved, in particular PI3K/Akt/mTOR and TGF-β1, which promote the synthesis of type II collagen and proteoglycans – key components of the extracellular matrix (ECM) of cartilage [3, 4, 8,18]. In animal models, increased expression of ECM components has been observed alongside a reduction in pro-inflammatory cytokines such as IL-1β and TNF-α [6, 8].
Clinical studies in humans
Human studies have so far focused primarily on clinical endpoints such as pain (e.g., VAS score), joint function (WOMAC, KOOS) and quality of life in knee osteoarthritis. Kumar et al. (2015) showed in a randomized double-blind study with patients that collagen peptide supplementation achieved significant improvements in these parameters compared to placebo [13]. Similar findings were confirmed in another study involving 99 patients who took collagen hydrolysate in addition to exercise therapy [14]. However, there is often no evidence of a structural or molecular biological mechanism in humans.
Proteolytic enzymes – inflammation control through systemic enzyme therapy?
The most common enzymes in dietary supplements for the treatment of osteoarthritis are:
- Bromelain: cysteine protease from pineapple stems
- Trypsin: serine protease from the pancreas
- Rutoside (a flavonoid): often found in combination preparations (e.g. Wobenzym®)
Enzyme therapy also raises the question of what actually reaches the knee: enzymes are proteins with a defined 3D structure, which is essential for them to perform their function. Proteases (such as bromelain and trypsin) recognize specific proteins in order to break them down. The fit between the enzyme and the substrate is as precise as a key and a lock, which means that denaturation of the enzymes, i.e., the loss of their 3D structure, leads to a loss of function. However, this is exactly what happens due to the hydrochloric acid and the protein-splitting pepsin in the stomach. Studies mention the use of enteric-coated tablets or liposomal encapsulation to enable passage into the small intestine [19]. However, proteases are also present in the small intestine, and here too, transport into the blood is not normally intended for such large molecules. Some evidence suggests that active fragments or peptide complexes enter the bloodstream and have an immunomodulatory effect there, but this is mostly indirect evidence. Nevertheless, numerous studies show the effectiveness of enzyme preparations in knee osteoarthritis, primarily in comparison to NSAIDs: Wobenzym (trypsin-bromelain-rutoside combination) was clinically non-inferior to diclofenac in several studies in terms of pain and functional parameters [20, 22]. Patient-reported side effects were lower, especially gastrointestinal complaints. In systematic reviews [23], bromelain was associated with direct anti-inflammatory effects on joint symptoms, partly comparable to NSAIDs. However, some studies, e.g. [21], found no statistically significant effects vs. placebo.
The anti-inflammatory mechanisms are described as follows, but there are no publications on this in standard medical journals:
- Reduction of pro-inflammatory cytokines: TNF-α, IL-1β, IL-6 are regulated by inhibition of signaling pathways such as NF-κB and MAPK [24, 25]
- Fibrinolytic effects: Bromelain and serratiopeptidase in particular dissolve fibrin and prevent vasoconstriction in microcirculation – potentially important in chronic inflammation
- Chondroprotection: Inhibition of cartilage-degrading enzymes (e.g. MMPs), promotion of cartilage cell viability
- (preclinical evidence shown in [24])
Significance and relevance of NEMs such as collagen and enzymes
Safety and long-term use: According to studies, both substance groups — collagen and enzymes — are well tolerated. Gastrointestinal side effects are less common than with NSAIDs. With enzyme therapy: nausea, diarrhea, or allergic reactions are rare.
Collagen: well tolerated, isolated cases of mild GI symptoms reported. Long-term data on structural joint preservation are limited, especially for enzymes.
Indications: Early stages of knee osteoarthritis (Kellgren-Lawrence I–II), especially symptomatic patients with contraindications for NSAIDs (e.g. GI ulcers), athletes or physically active individuals who wish to support their joint function prophylactically
Limitations: Individual response variability, depending on factors such as age, metabolism or gut microbiome. Regulatory gray area for dietary supplements: Dosages and quality are not standardized as they are for drugs.
Conclusion
Both hydrolyzed collagen peptides and systemically active enzymes have been shown in studies to have positive effects on pain and function in knee osteoarthritis — some of which are comparable to NSAIDs, but with better tolerability. Although the scientific evidence is promising in many respects, particularly for collagen, it is not yet fully clarified. In the future, better data on bioavailability, long-term effects, and individualized application will be necessary.
Literature
[1] Welsch, U. (2022) Histologie – Lehrbuch und Atlas, 6. Auflage, Elsevier
[2] Fluhrer und Hampe (2023), Biochemie hoch2, 2. Auflage, Elsevier
[3] Isaka S et al. (2017) Evaluation of the effect of oral administration of collagen peptides on an experimental rat osteoarthritis model Experimental and Therapeutic Medicine 13 (6), 2699-2706
[4] Ohara H et al. (2010) Effects of Pro-Hyp, a collagen hydrolysate-derived peptide, on hyaluronic acid synthesis using in vitro cultured synovium cells and oral ingestion of collagen hydrolysates in a guinea pig model of osteoarthritis Bioscience, Biotechnology, and Biochemistry 74 (10), 2096-2099
[5]Iwai et al. (2005) Identification of food-derived collagen peptides in human blood after oral ingestion of gelatin hydrolysates Journal of Agricultural and Food Chemistry 53 (16), 6531-6536
[6]Felim J et al. (2022) Effect of Different Collagen on Anterior Cruciate Ligament Transection and Medial Meniscectomy-Induced Osteoarthritis in Male Rats Frontiers in Bioengineering and Biotechnology 10, 917474
[7]Oesser S et al. (1999) Oral administration of (14)C labeled gelatin hydrolysate leads to an accumulation of radioactivity in cartilage of mice (C57/BL) The Journal of Nutrition 129 (10), 1891-1895
[8] Lee MH et al. (2021) Low-Molecular-Weight Collagen Peptide Ameliorates Osteoarthritis Progression through Promoting Extracellular Matrix Synthesis by Chondrocytes in a Rabbit Anterior Cruciate Ligament Transection Model Journal of Microbiology and Biotechnology 31 (10), 1401-1410
[9] Dar QA et al. (2017) Daily oral consumption of hydrolyzed type 1 collagen is chondroprotective and anti-inflammatory in murine posttraumatic osteoarthritis PLOS ONE 12 (4), e0174705
[10] Schadow S et al. (2017) Metabolic Response of Human Osteoarthritic Cartilage to Biochemically Characterized Collagen Hydrolysates International Journal of Molecular Sciences 18 (1), 207
[11] Nakatani S et al. (2009) Chondroprotective effect of the bioactive peptide prolyl-hydroxyproline in mouse articular cartilage in vitro and in vivo Osteoarthritis and Cartilage 17 (12), 1620-1627
[12] Sudirman S et al. (2023) Fermented jellyfish (Rhopilema esculentum) collagen enhances antioxidant activity and cartilage protection on surgically induced osteoarthritis in obese rats Frontiers in Pharmacology 14, 1095665
[13] Kumar S et al. (2015) A double-blind, placebo-controlled, randomised, clinical study on the effectiveness of collagen peptide on osteoarthritis Journal of the Science of Food and Agriculture, 95(14):2767–2772
[14] Repetyuk AD et al. (2023) Effectiveness of a novel hydrolysate collagen formulation in the complex treatment and rehabilitation of patients with symptomatic knee osteoarthritis Medical and Social Expert Evaluation and Rehabilitation 26(1):1–10
[15] Ohnishi A et al. (2013) Evaluation of the chondroprotective effects of glucosamine and fish collagen peptide on a rabbit ACLT model using serum biomarkers The Journal of Veterinary Medical Science 75(4):555–561
[16] Schadow S et al. (2013) Collagen Metabolism of Human Osteoarthritic Articular Cartilage as Modulated by Bovine Collagen Hydrolysates PLOS ONE 8(1):e53955
[17] Schunck M et al. (2017) The Effectiveness of Specific Collagen Peptides on Osteoarthritis in Dogs-Impact on Metabolic Processes in Canine Chondrocytes Open Journal of Animal Sciences 7(3):254–266
[18] Geahchan et al. (2022) Marine Collagen: A Promising Biomaterial for Wound Healing, Skin Anti-Aging, and Bone Regeneration. Marine Drugs. 10;20(1):61.
[19] Kulkarni, A. & Bendrey, H.A. (2021) Systemic enzyme therapy with trypsin, bromelain and rutoside in the management of arthritis: an overview. International Journal of Research in Orthopaedics. 7(5):1062-1069
[20] Bolten, W., Glade, M.J., Raum, S., Ritz, B., & others. (2015) The Safety and Efficacy of an Enzyme Combination in Managing Knee Osteoarthritis Pain in Adults: A Randomized, Double-Blind, Placebo-Controlled Trial. Arthritis. 2015:251521
[21] Brien, S., Prescott, P., Lewith, H., Walker, A., & Bundy, R. (2006) Bromelain as an adjunctive treatment for moderate-to-severe osteoarthritis of the knee: a randomized placebo-controlled pilot study. QJM: An International Journal of Medicine 99 (12), 841-850.
[22] Ueberall, M., Maier, C., Schuler, M., Essner, U., & Bonninger, K. (2016) Efficacy, tolerability, and safety of an oral enzyme combination vs diclofenac in osteoarthritis of the knee: results of an individual patient-level pooled reanalysis of data from six randomized controlled trials. Journal of Pain Research 9, 877–885.
[23] Savadjani, S.A., Jahanbani-Ardakani, H., Seyednozadi, S., & Khaghani, A. (2023) The effects of bromelain on osteoarthritis symptoms: A systematic review. Journal of Shahrekord University of Medical Sciences 25(2), 55-65.
[24] Pothacharoen, P., Kongtawelert, P., Phitak, T., Suttisansanee, U., Teanpaisan, R., & Vaithanomsat, P. (2021) Bromelain Extract Exerts Antiarthritic Effects via Chondroprotection and the Suppression of TNF-α–Induced NF-κB and MAPK Signaling. Plants 10 (7), 1385.
[25] Nobre, T.A., Costa, R.d.C., Cavalcante, R.V., Lima, L.F., da Silva, G.S., & Torres–Leal, F.L. (2024) Bromelain as a natural anti-inflammatory drug: a systematic review. Natural Product Research 38 (4), 1855-1865.
Autoren
ist Dozentin der Stoffwechsel-Biochemie an der LMU in München. Ihr Schwerpunkt sind die klinischen Bezüge im Stoffwechsel: Ernährung und Nahrungsergänzungsmittel (NEM) sind hier Kernthema. Als Autorin des Biochemie hoch2 Buchs von Elsevier hat sie unzählige klinische Fallbeispiele verfasst. Aktuell arbeitet sie an einer sportmedizinischen Publikation für die Vorklinik, bei der Ernährung und NEM bei verschiedenen Sportarten beleuchtet werden.