Myofascial trigger points are palpable areas of muscular hardening, usually in the neck or between the shoulder blades, which may be associated with considerable impairment of the quality of life.
Due to pain in the region of the shortened musculature and the associated stiffness of the affected mobile segments, e.g. the atlanto-occipital and atlantoaxial joints in the cervical spine or the shoulder, the further course may lead to postural imbalance in more distant joints (ascending/descending chain) and to chronified pain syndromes that often have to be treated with drugs. One can differentiate between active myofascial trigger points that are frequently extremely painful and often weaken the affected muscle, latent myofascial trigger points that are only painful on movement, and associated myofascial trigger points that develop due to dysfunction of the neighbouring muscle groups.
In many cases the latter myofascial trigger points are areas of painful muscular tension in the muscles of the shoulder (girdle) (rhomboideus major/minor muscles) that react to muscular shortening, particularly at the superior border of trapezius or in the short cervical muscles. The causes of trigger points are many and varied: shortening of the muscle groups due to damp/cold/draughts, associated fascial adhesions, postural imbalance, overstrain, or blunt trauma. Imaging has only been of very limited use for trigger points to date. Many patients with chronified neck problems show no structural anomalies on imaging (MRI, digital volume tomography, radiographs of the cervical spine). Ultrasonography is also only of limited use for assessing trigger points.
A dedicated manual examination gives indications of shortened muscle groups. Intensive examination of the ranges of movement of the atlanto-occipital and atlantoaxial joints often reveals muscular swelling at palpation. More recently clinicians have been turning their attention to thermography because this specific examination system can demonstrate hyperaemia in the affected muscular segment. Thus, for the first time ever, trigger points can be visualised without exposure to radiation, relatively problem-free, and in a short time.
Case example
A young athletic woman presented at our surgery with progressive recurrent episodes of symptoms in the region of her left trapezius radiating cranially to the left occipital area that she had had for several weeks. She said she did sports regularly (tennis).The patient is right-handed and could not remember any trauma. She has a sedentary occupation (works at a computer). Her intensive stress situation had worsened over the last few weeks as she had had to take on additional work due to staff reductions as a result of coronavirus. She had treated herself with deep heat, massage and analgesic gels. Clinical examination showed marked elevation of the left shoulder with massive tension of the superior border of trapezius and considerably restricted mobility of the atlanto-occipital and atlantoaxial joints on right rotation. She had tenderness to pressure over the insertions of the short cervical muscles on the occiput and along the course of the left levator scapulae muscle. Palpable myogeloses / trigger points, particularly at the superior border of trapezius and in the rhomboideus minor muscle.
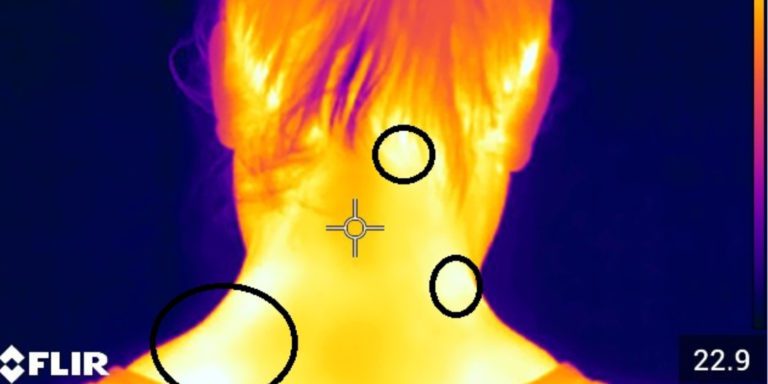
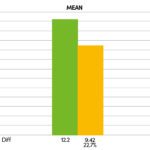
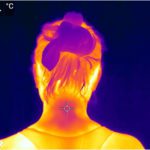
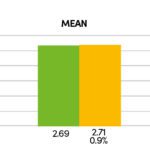
Slight pain relief in the affected muscle groups on extension of the neck. Clinical examination revealed no attributable radiculopathies. The MRI of the cervical spine the patient brought with her showed findings in the cervical spine that were compatible with her age without any higher-grade degenerative changes of the facet joints/intervertebral discs. No neuroforaminal narrowing. In the infra-red thermography we initiated (FLIR E75 thermal imaging camera, Fig. 1) the camera displays more than 75,000 measuring points with a thermal sensitivity of < 0.04 degrees temperature difference, and can thus accurately demonstrate small areas of hyperaemia (trigger points). In the present case the clinically diagnosed trigger points in the region of the superior border of trapezius and in the short right cervical muscles are shown (Fig. 2, see black circles). In order to confirm the diagnosis further we also ran EMG tests on the muscles in the shoulder girdle that gave clear evidence of elevated resting tone in the left trapezius (Fig. 3 and 4). Therapy was given at the same sitting as treatment with neuroreflex cryotherapy (Cryolight). With the help of the applicator and a temperature probe, the entire muscle area (in this case the trapezius on the left) is “cooled down”. During the treatment, the entire trapezius muscle is treated from the shoulder area to the area of the short neck muscles for approx. 60 – 90 seconds and then a dosed stretching treatment is carried out. The total duration of therapy per session is a maximum of 2 minutes. Depending on the intensity of the symptoms, 3 – 5 sessions are usually necessary (Fig. 5). Taping was then applied (Fig. 6). The thermography we repeated directly after the cryotherapy showed marked regression of the size of the pre-existing left nuchal trigger points (Fig. 7). In the further course the follow-up (EMG) examination also showed a marked reduction of the imbalance with clear harmonisation of muscle tone (Fig. 8). The patient’s treatment was repeated once. After the second sitting (six days after the first treatment session) there was almost complete regression of the symptoms with a considerably improved range of movement and no residual muscular limitations.
Summary
Thermal imaging (thermography) readily demonstrates trigger points – especially in the region of the cervical spine – with associated muscle weakness, restricted mobility and chronified pain syndrome. The application of cryotherapy is recommended for confirmed trigger points (neuroreflex cryotherapy) followed by taping. Furthermore, EMG testing (with concomitant biofeedback training) can be used for further diagnostics/treatment or used to evaluate the outcome of cryotherapy. Our EMG tests showed a marked reduction of muscular tension after cryotherapy indicating in summary that this technique, which is simple to apply, is a fast-acting form of treatment and is virtually free of side effects.
Autoren
ist Leiter von Ortho4Sport in Köln. Er ist Facharzt für Chirurgie mit Zusatzbezeichnungen Sportmedizin und Chirotherapie. Außerdem ist Professor Tobolski Verbandsarzt des Tennisverbandes Mittelrhein sowie ATP-Turnierarzt.