The use of adipose derived stem cell therapies are still up for debate, but are no longer a future vision of just some credulous medical scientists. In recent years this former vision seems to turn into reality. Among the numerous potential application areas of adipose derived stem cell therapies, the treatment of damaged tissues after athletic injuries as well as the therapy of degenerative diseases such as osteoarthritis (OA) is one hot topic.
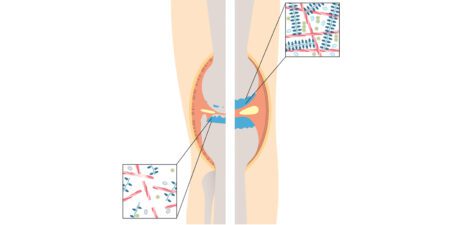
OA is a degenerative joint disease, which mainly affects the articular cartilage and belongs to the ten most disabling diseases in developed countries. Several treatment options are available for OA, with different benefits and risks [1, 2]. To further evaluate the potential value of stem cell therapy for OA, our team performs an ongoing data collection using a new, unique biological treatment option. Regenerative cells such as adult stem cells from adipose tissue (ASCs, adipose-derived stem cells) are used in combination with a leukocyte poor PRP autologous conditioned plasma (ACP). The interest in the potential therapeutic value of ASCs for regenerative medicine has been generated through their multipotency and the capability to secrete a large number of cytokines and growth factors [3 – 6]. A further advantage for clinical applications is the easy harvest and abundance of ASCs. They are part of the stromal vascular fraction (SVF), that can be isolated easily, effectively and fast from adipose tissue through liposuction and the following processing of the aspirate. The technique is based on the mechanical dissociation of the mature adipocytes leaving behind the pelleted SVF. The resulting SVF-pellet consists of a heterogeneous cell population. Besides the ASCs also includes hematopoetic cells, pre-adipocytes, pericytes, endothelial and progenitor cells [5]. By now several in vivo studies, using animal and cell culture models, have proven the safety as well as immunosuppressive, anti-oxidative, antiapoptotic and angiogenic properties of SVF cells and ASCs [7 – 14]. Due to the possible regenerative potential, first preclinical and clinical tests to treat osteoarthritis with autologous SVF have been conducted. The published results confirm the previous hypothesis of a healing effect [15 – 17].
In order to further improve the treatment efficiency of SVF/ASCs, a new approach is to combine them with leukocyte poor platelet-rich-plasma (PRP). Leukocyte poor PRP is obtained easily from whole blood through centrifugation. The red blood cells and the majority of leukocytes are removed and the platelets in the plasma are concentrated. Thereby growth factors, that are released by the platelets are enriched [18]. The field of application is huge and in the past included chronic tendinitis, osteoarthritis, plastic surgery and bone repair and regeneration [17, 19 – 22]. Specifically when used to treat mild to moderate OA it was shown in several level I studies that leukocyte PRP leads to a significant better clinical outcome compared to hyaluronic acid or placebo [23 – 26]. By combining ASC with leukocyte poor PRP we hypothesize, that the number of injections can be reduced and the clinical outcome can be further improved. In several in vitro and preclinical studies it has been shown that PRP and ASCs have a synergistic effect. It could be demonstrated that PRP promotes cell proliferation and differentiation of adipose-derived stem cells in different tissues such as cartilage, bone and skin [27 – 32]. The great potential of the regenerative match ACP and SVF has been shown by Loibl et al. in vitro and through first successful treatments of osteoarthritis with SVF plus PRP [29, 33, 34]. At our clinic we treated so far 18 knee osteoarthritis patients with ACPSVF. Here we present the first results gathered over a three month follow-up.
Material and Methods
For production of the SVF the Adipose Tissue Harvesting Kit in combination with ACP Double Syringes was used. For liposuction 60 ml of tumescence solution was infiltrated into the target area (either abdominal wall or thigh). After a waiting period of 15 min 30 ml of adipose tissue was harvested into 2 ACP double syringes, 15 ml each using the harvesting cannula from the Adipose Tissue Harvesting Kit. Both ACP double syringes were centrifuged for 4 min at 2.500 rpm in the appropriate centrifuge resulting in a three layer separation of the lipoaspirate. Using the double syringe principle, the oil and aqueous fractions were removed, leaving the fat graft behind (Figure 1). The fat graft was swooshed at least 30 times through the swooshing device for mechanical dissociation of the adipocytes. Following a second centrifugation at 2.500 rpm for 4 min the separated oil was removed leaving the SVF (cell pellet) in the ACP Double Syringe (Figure 2).

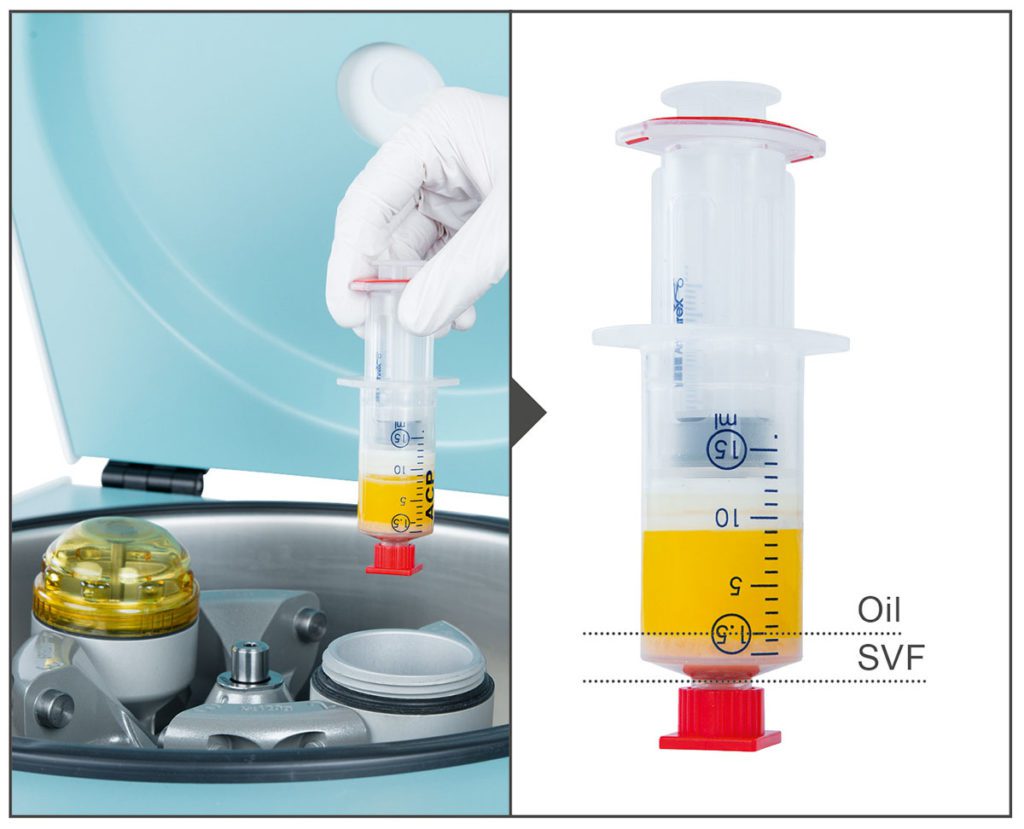
For production of ACP 15 ml of venous blood was withdrawn directly into the ACP Double Syringe and centrifuged for 5 min at 1.500 rpm using the centrifuge Rotofix 32A. Following the centrifugation process the supernatant ACP was transferred from the larger outer syringe into the small inner syringe. Before usage the small inner syringe was unscrewed and the ACP was ready for use at the point of care. Subsequently, ACPSVF was created by re-suspending the SVF cell pellet in ACP (Figure 3). Injections were performed by standard intra articular injection technique.

Patients were evaluated over a three month time period after therapy in terms of pain, stiffness and physical functionality via the VAS (Visual Analog Pain Scale) and WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index); both valid, reliable and widely used scores to evaluate the conditions of patients with osteoarthritis of the knee. Scores were collected at set time points via
the online Surgical Outcomes System (SOS) (Arthrex, Naples, FL). SOS is a global registry for orthopedic/trauma surgery and sports medicine. With the web-based platform, surgical procedures and treatment results can easily recorded, viewed and assessed. For the recording of the data the patient receives an e-mail questionnaire at the specified time points which he/she then completes.
Results
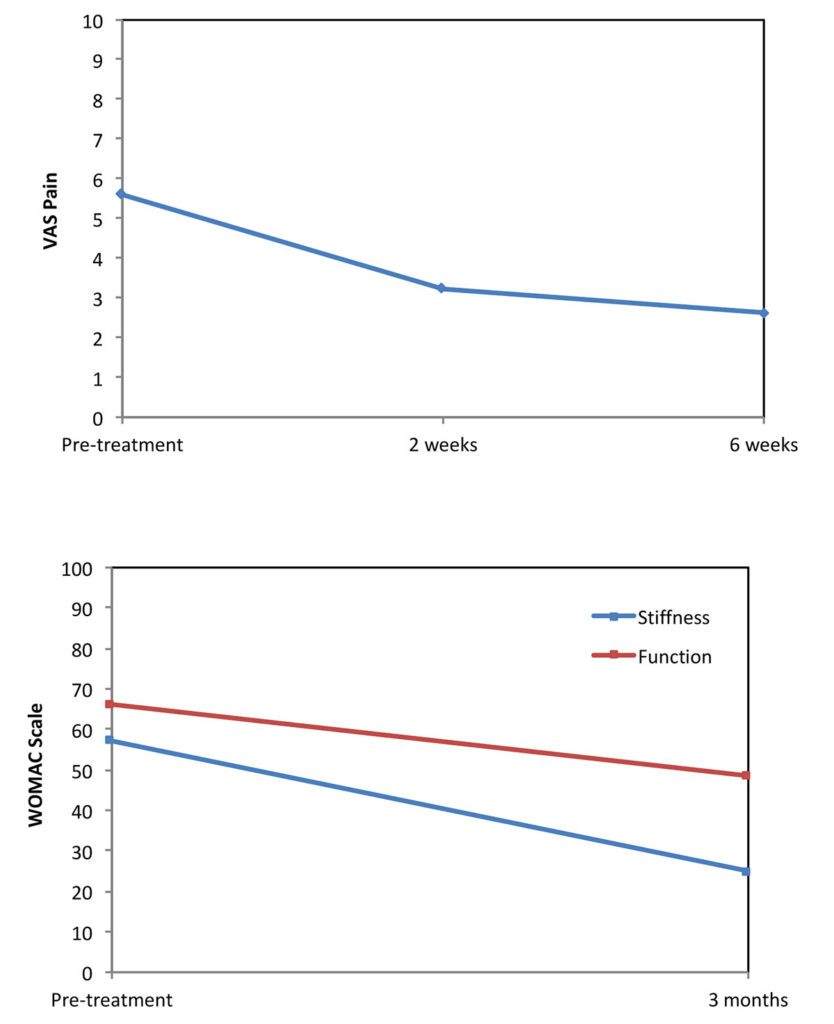
Our purpose of the ACPSVF application is to decrease the pain and to increase the physical functionality of patients with knee osteoarthritis. Overall we treated 18 knee osteoarthritis patients (age between 43 and 77) with ACPSVF either during a knee arthroscopy or through a non-surgical application. To measure the patient’s pain intensity we used the common pain scale VAS (Visual Analog Pain Scale). The VAS scale ranges from 0 – 10, in which 10 reflects an extreme and 0 no pain. The patients were asked for their pain before as well as two and six weeks after the treatment with ACPSVF via the online Surgical Outcomes System. For the final evaluation, the mean values of the VAS scores of all participating patients were calculated. As shown in Figure 4 the patients started with a mean pain level. Already two weeks after the treatment with ACPSVF the pain could be reduced by 50 percent and six weeks after the treatment it decreased even further.
Furthermore we used the WOMAC score (Western Ontario and McMaster Universities Osteoarthritis Index) to analyze the stiffness of the knee joint and the physical function in regard to daily activities such as stair use, rising from sitting or doing light household duties. Similar to the VAS higher scores on the WOMAC indicate worse stiffness and functional limitations. The patients were asked to fulfil out the questionnaire before as well as three months after the treatment with ACPSVF via the online Surgical Outcomes System. Figure 5 shows the mean values of the WOMAC scores of all participating patients. Both the stiffness and the function could be improved over a time period of 3 months. However the improvement of the stiffness is much clearer than of the functionality. Besides the positive effects of ACPSVF in terms of pain, stiffness and functionality of patients with knee osteoarthritis, we did not find any adverse events. In addition to the effectiveness, this also confirms the safety of this new biological treatment option for osteoarthritis.
Discussion
Osteoarthritis is one of most common adult joint diseases worldwide. We treated patients suffering from knee osteoarthritis with a new, unique biological treatment option. ACPSVF combines the regenerative potential of adult stem cells from adipose tissue with the benefits of leukocyte poor PRP autologous conditioned plasma. Our first results could confirm the promising potential of this regenerative match for the treatment of osteoarthritis. Overall 18 patients were treated with ACPSVF. The pain of the patients was evaluated two and six weeks after the treatment with the VAS score, as well as stiffness and physical function of the knee after 3 months with the WOMAC. Within this short period of time the patients showed an impressive improvement compared to their initial state in all categories, pain, stiffness and function. Importantly we did not find any adverse events during or after the treatment with ACPSVF. However, despite the first success of ACPSVF, further evaluation of the long-term safety is important.
An additional advantage of ACPSVF is the need of less fat tissue that has to be harvested comparing to other systems. Especially in athletes, who usually have very little fat, this might be a great benefit. Furthermore less trauma of tissue is caused by harvesting and the preparation process is very easy and fast. We belief ACPSVF is safe and provides quantifiable benefits for pain relief and functional improvement in regard to knee OA. Because of the satisfying handling and the results of ACPSVF, we now have extended the treatment to other fields of application. In individual patients ACPSVF was injected into the patellar tendon, the shoulder or the hip for example. We are convinced that these patients will also benefit from this treatment and their quality of life will increase again.
Autoren
Orthopedic surgeon working in the field of sports medicine with deep focus on orthobiology, and cartilage repair. He is Head of Clinic, LEKMED, Warsaw, since 2013. Treatment of patients with sports related injuries, osteoarthritis. Currently working at Gamma Clinic (partner of LEKMED Clinic since 2016). Also Dr. Slynarski is Founder and Vice President of the Polish Arthroscopic Society.