Health starts in the cells. Basic scientific studies have shown that nuclear magnetic resonance therapy (KSRT = Kernspinresonanz-Therapie, NMRT = nuclear magnetic resonance therapy, tNMR = therapeutic nuclear magnetic resonance, MBST®) can address cellular processes that are also relevant to musculoskeletal conditions and injuries on several levels.
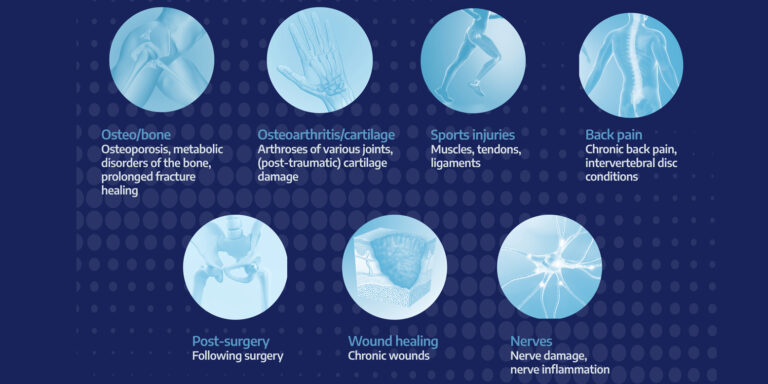
NMRT can, among other things, modulate circadian rhythms or the cellular clock, hypoxia signaling pathways (HIF-1α), and mitochondrial metabolism based on quantum biology, reduce inflammation markers, and activate regenerative signaling pathways. In addition, NMRT has been shown to promote nerve regeneration in animal models, contribute to regenerative cell proliferation in-vitro (e.g., chondrocytes, osteoblasts), and improve the conditions of the extracellular matrix3. The therapeutic effect of this unique combination of magnetic fields and radiofrequency sequences appears to be more effective than the individual components. Physiological regeneration processes can thus also be supported in a targeted and even tissue-specific manner with this physical therapy modality. Symptoms can be alleviated and, in many cases, the pathology can also be addressed causally. Magnetic resonance therapy is increasingly being used worldwide by therapists in various practice settings, but also by sports clubs for various indications and tissue types in cases of complaints, injuries, and painful, degenerative, and / or pathological changes in the musculoskeletal system (Fig. 1) as part of multimodal therapy1, 2. The clinical-scientific collaborations consist of international cooperation between universities, clinics, and practices, as well as professional sports clubs such as HSV and Wrexham AFC. In addition to practical clinical experience from over 20 years of MBST® with various case reports and company vigilance data, the clinical data also includes current reviews and older retrospective and prospective data collections, primarily in the areas of back pain, osteoarthritis, and osteoporosis (Clinical Evaluation Report, 2022). The table below provides a summary overview of the most relevant clinical data on magnetic resonance therapy. In summary, clinical study data show that NMRT leads to good pain reduction in osteoarthritis, contributes to an increase in bone density in osteoporosis, reduces sick days in back pain, and can improve the rehabilitation effect, e.g., due to pain reduction.
Further research and, above all, more clinical studies are needed in order to further integrate NMRT into existing therapy concepts and to underpin it with more clinical evidence.

Empirical values from practice
Dr. Stephan Hub has many years of experience with magnetic resonance therapy (NMRT) in his practice, where he sees patients with statutory health insurance, private health insurance, and occupational accident insurance, and performs both surgical and conservative treatments. He has treated numerous patients with this therapy. NMRT is a good option if the indications are in the area of conservative treatment, the patient does not want surgery or is not yet ready for it, or decides against it again based on previous positive experience with MBST®. Based on his experience, these are the most common areas of application for NMRT as part of his combination therapy:
Osteoarthritis (using the example of knee osteoarthritis)
Patients typically experience pain during weight-bearing activities, often accompanied by effusion and restricted movement in the affected knee joint. According to the Kellgren and Lawrence classification system used in X-ray diagnostics, stage I is treated with physiotherapy and muscle-building exercises, as well as NSAIDs if necessary. In stages II and III, in addition to the above-mentioned therapy options, regenerative measures are carried out, which include autologous conditioned serum (ACS) and hyaluronic acid administration, as well as NMRT. In stage IV, in addition to supportive hyaluronic acid injections, TKA is indicated depending on the severity of the symptoms.
Osteoporosis
Patients often present with nonspecific back pain and/or osteoporosis-related fractures, or therapy is planned accordingly after a diagnosis of reduced bone density using osteodensitometry. After detailed consultation and consideration of all treatment options, patients often decide to undergo NMRT, either alone or in combination with guideline-based drug therapy, the potential side effects of which are known, accompanied by physiotherapy and an adapted diet.
Delayed- / Non-unions / fractures
Here, it has been shown that delayed fracture healing (delayed to non-union/pseudarthrosis), “problem fractures” such as subtrochanteric femoral fractures, scaphoid fractures, complex bone fractures such as tibial plateau fractures or calcaneal fractures, and osteoporotic vertebral fractures also benefit from NMRT as an adjuvant conservative treatment and postoperatively. In the above setting, this is usually combined with shock wave therapy (ESWT), ultrasound, and a nutritional concept.
Tendinopathies / insertional tendinosis
NMRT has proven effective in combination with physiotherapy (PT) (eccentric training/stretching), ESWT, and ACS for classic diagnoses such as tennis elbow and golfer’s elbow, as well as heel spurs and runner’s and jumper’s knee.
Wounds
NMRT can also be used to complement classic wound treatment. In particular, burns, but also chronic diabetic ulcers show good treatment success here.
Spinal disorders
Here, NMRT proves to be a useful supplement, especially for degenerative diseases of the spine, but also for conservatively treated herniated discs in combination with PT, Powerspine, and a nutritional concept. However, due to the pathology, it is often necessary to use two cards for different tissue types, i.e., 2 x 7–10 hours of therapy sessions.
Autoren
ist Facharzt Orthopädie und Unfallchirurgie. Er ist Chefarzt der Abteilung Orthopädie und Unfallchirurgie am Krankenhaus Ingelheim und ist im Team der Unfall-/Chirurgischen Gemeinschaftspraxis Am Brand in Mainz (Janocha/ Özay/Hub). Seine Schwerpunkte sind orthopädische Gelenkchirurgie und Endoprothetik, Verletzungen des Muskoloskelletalen Systems sowie ambulante und stationäre Operationen. Außerdem ist Dr. Hub wiss. Beirat der sportärztezeitung.
ist Fachärztin für Orthopädie und Unfallchirurgie. Sie war jahrelang an renommierten Kliniken tätig, absolvierte ein Research Fellowship in den USA und war u.a. auch Sektionsleiterin Wissenschaft des Jungen Forums O&U. Sie wechselte dann in die Industrie und ist aktuell als Chief Medical Officer bei der MedTec Medizintechnik GmbH tätig. Sie lehrt weiterhin an der Eberhard Karls Universität Tübingen bzw. der dortigen Orthopädischen Universitätsklinik und ist Dozentin der AKAD.